veterinary renal diets
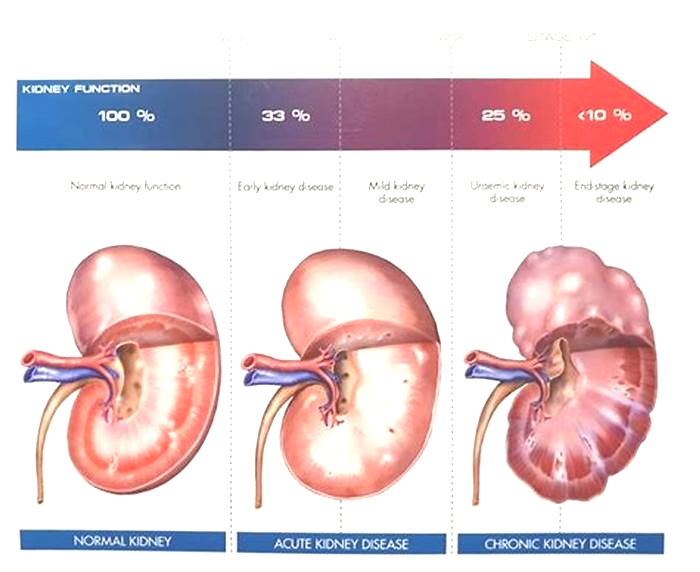
Many aspects of kidney failure require attention. The goal of renal therapy, dietary or otherwise, is to prevent or at least postpone advanced uremia (poisoning by toxins the kidneys could not adequately remove) and extend life expectancy and quality.Diet is an important part of achieving these goals and we are lucky to have commercially available diets made specifically for renal patients.
The idea behind using diet as therapy for kidney disease involves making alterations in the patient's diet to correct or at least dampen the toxic metabolic state of kidney failure. A modified diet can thus be used to correct imbalances and slow progression of disease while maintaining a healthy muscle mass and body condition.
In one famous study where 38 dogs in kidney failure were tracked for 2 years, dietary therapy reduced the risk of dying by 69% over dogs allowed to continue eating regular dog food.
Another study in dogs showed that beginning the renal diet when the creatinine was between 2.0 and 3.1 delayed the onset of uremic crisis by 5 months.
A study of 50 cats with stable, naturally occurring renal failure were divided into two groups, one receiving a renal diet and the other receiving regular food. The cats on the renal diet survived over twice as long as the others.
There are more studies where these came from showing great survival and life quality benefit for renal patients who eat renal diets rather than regular maintenance diets.
What Makes a Renal Diet Different?
A renal diet takes into consideration reduction in uremic toxins, control of high blood pressure, calcium/phosphorus balance, maintenance of proper potassium levels and reduction in inflammation. Let's review the features of a renal diet and why they are important:
Kibble Cat Food

Photo Courtesy Dr. Teri Ann Oursler
Phosphorus Restriction
This is an important part of a renal diet since phosphorus balance is crucial. Phosphorus comes into the body through the diet and leaves it through the kidney. The problem is that when kidney function is poor, not as much phosphorus is removed as needs to be.
Obviously using less phosphorus in the diet may be enough to keep the blood phosphorus levels normal, thus balancing the intake with the output, but sometimes addition of medication (i.e. a phosphate binder) is needed to further reduce intake. Restricting dietary phosphate has been shown to slow the progression of renal disease.
If the goal phosphorus level has not been achieved in4 to 6weeks after starting the renal diet, a phosphorus binder should be used.
Potassium Supplementation
In chronic kidney disease, potassium is not conserved properly and becomes depleted. When potassium depletion becomes excessive, the patient's overall muscle strength, energy and general life quality are affected. Potassium supplements may be needed in the form of oral gels or powders but ideally, potassium is supplemented in the easiest possible way which generally means incorporating more potassium in the diet. If potassium levels can be maintained simply with food, this would mean less medication for the patient to have to take.
Omega 3 Fatty Acids
Studies suggest that kidney failure patients taking omega 3 fatty acids are likely to live longer than patients who do not take them. This has led to the supplementation of most renal diets with fish oils. The full import of fatty acid supplementation is still being worked out.
Other dietary features include B vitamin supplementation (since the damaged kidneys tend to lose excess B complex), which have non-acidifying features to help control acidosis.
Low Protein?
Since a number of renal toxins come from the break-down and processing of protein, one way to give the kidneys less work to do is to eat less protein. How much less protein depends on how serious the kidney disease is as there is a minimum protein requirement for maintaining body condition and a protein-restricted diet must not be restricted below that level.
Exactly how to restrict protein involves a lot of choices. Older animals tend to require a higher dietary protein level in general when compared to their younger counterparts. Protein also adds palatability to the food so that if we try to restrict protein too much we may end up with a pet who will not eat at all. Further, plant proteins tend to produce less difficulty with phosphorus balance but animal origin proteins may be needed for required amino acids. It is no surprise that decades of research have gone into how protein selection is accomplished to create an effective but tasty diet.
- There is no protective value to restricting protein prior to the onset of kidney failure. It is not preventive or at all helpful for a healthy senior pet to be restricted in dietary protein.
- High-protein diets do not cause kidney failure (though they certainly make the patient worse after kidney failure has begun).
- Protein restriction is probably the least important dietary modification in early stages of kidney disease. There are special diets available for patients with less restrictive needs and others for patients in more advanced states.
At What Point Should a Special Diet be Started?
This questionhas been controversial for a long time. For many animals, changing diet to a less palatable food represents a definite reduction in life quality. There was some thinking that weare changing the diet too soon. On the other hand, if a pet is in a more advanced state of disease before the switch is made, the pet will be much less willing to change to a food of less palatability. The companies that make these foods have put a great deal of research into improving palatability over the years, which has helped tremendously.
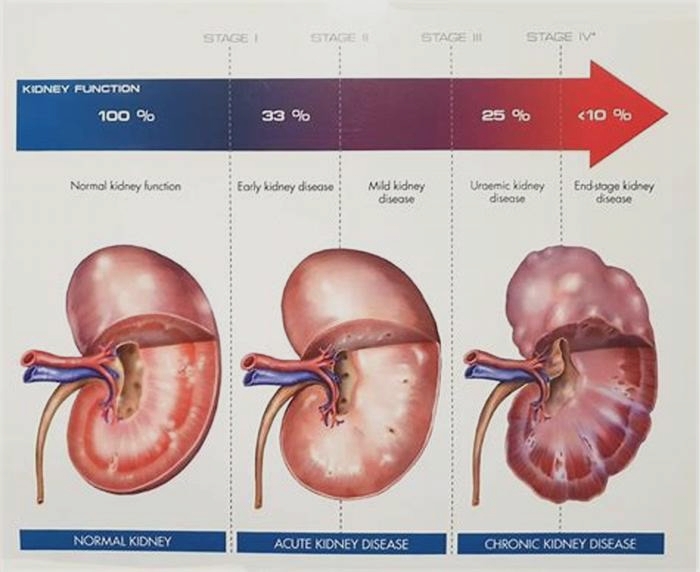
Now the International Renal Interest Society finally has guidelines.
The IRIS Guidelines recommend considering a change to a renal diet by IRIS Stage II (creatinine test between 1.6 mg/ml and 2.8 mg/ml with an SDMA test between 18 & 25 in cats; creatinine test between 1.4 mg/ml and 2.8 mg/ml with SDMA test of 18 & 35 for dogs). The diet should have clear benefits at IRIS stage III which is later on, but the recommendation has been moved to a lower stage because animals in stage III are less likely to accept diet change. It was deemed that the change should be made earlier to have a better chance to be in place when it is more crucially needed.
These guidelines allow the patient to benefit the most from the preventive advantages of the diet. If the pet finds the diet palatable, then there should be no life quality issues with changing foods.
What if my Pet Will Not Eat the Renal Diet?
Animals with insufficient kidney function frequently do not feel well and will not be inclined to eat bland food. Here are some tips in increasing acceptance of renal diet.
Is the Pet Feeling Iill?
As mentioned, the pet that feels ill may be disinclined to eat a new food. Consider using other medical treatments until the pet is feeling better before changing diets.
Orange Cat on Desk

Photo Courtesy Dr. Teri Ann Oursler
Consider Feeding Access
If the pet feels ill, he or she may not feel like walking across the house to the feeding area. Be sure the food is accessible.
Offer a Choice of Renal Diets
At this point, there are many renal diets available in different textures and different flavors. There are kibbled foods, stews, morsels and gravy, pates, and loaf formats. Commonly a renal patient will eat one food for a while and then stop accepting it only to accept a new format, even if it was rejected on a prior location. Your vet can help you get a selection so that even a picky pet find something acceptable.
Appetite Stimulants/Medications
Medications such as capromorelin, mirtazapine or cyproheptadine can be used to enhance hunger and encourage eating.
If the pet simply does not respond, it may not be possible to use a renal diet and other medications may be needed (as reviewed in other areas of our Kidney Failure Center) to provide therapy.
If the patient is simply too sick to eat at all, assisted feeding may be in order.
Home Cooking a Renal Diet
Home cooking an appropriate renal diet is a complicated task as might be surmised from the information above. Commercial diets have decades of research behind them as well as government regulation and professional quality control. They are also convenient to use. That said, some pet owners prefer to have more control over the ingredients they feed their pets and want more involvement with diet choices. Commercial diets tend to represent a "one size fits all" approachthat may not be best.
For renal patients, it is important not to simply try to make up your own diet based on recipes from non-professional sources. Many recipes float around the internet and many pet owners may support them but this is not the same as getting guidance from a nutrition professional.Your regular veterinarian can guide you to an appropriate service for nutritional consultation. or you may wish to visit the American College of Veterinary Nutrition.
Renal diets for veterinary patients: What to feed and when to start
Getty ImagesAs one of the most amenable medical conditions to dietary management, renal disease in dogs and cats can be slowed, uremic episodes can be prevented, and patient survival time can be doubled when patients are fed specially formulated renal diets.1,2 Dietary modifications for chronic kidney disease (CKD)--restricted phosphorus, protein and sodium--help mitigate many metabolic changes that occur secondary to decreased renal function. Renal diets also promote alkaline urine production and usually contain B vitamins and omega-3 fatty acids.
Phosphorus
The most critical nutritional modification in patients with renal disease is phosphorus restriction. A number of well-designed studies have shown that controlling blood phosphorus concentration through dietary modification slows the progression of CKD. Reduced glomerular filtration rate (GFR) in CKD leads to decreased renal excretion of phosphorus. Hyperphosphatemia in turn leads to increased secretion of parathyroid hormone, leading to increased release of calcium and phosphorus from bone. Soft tissue mineralization, renal damage progression and marked bone loss are potential consequences.
The International Renal Interest Society (IRIS) has published guidelines on phosphorus management for renal patients. Because increased parathyroid hormone secretion can occur when serum phosphorus concentrations fall within the reference intervals,3 it's important to note that all the target serum phosphorus concentrations in the IRIS guidelines fall in the low to middle range of most laboratory reference intervals. As renal disease advances, it's often impossible to maintain phosphorus within the IRIS guidelines' target concentrations using diet alone. In these cases, use phosphate binders in addition to the lowest-phosphorus diet appropriate for the patient.
Keep in mind that nearly all diets for dogs and for cats labeled with the statement "formulated to meet AAFCO nutrient profiles" (i.e., primarily over-the-counter (OTC) maintenance or other diets) contain more phosphorus than is recommended for patients with all but the earliest of renal disease.
Protein
Reducing dietary protein is probably the best known and most controversial nutritional modification for patients with renal disease. No evidence exists demonstrating that high-protein diets harm the kidneys per se. However, nitrogenous compounds build up in the bloodstream when GFR is markedly compromised, and decreasing dietary protein can reduce the effects of these toxins on other systems, thus improving patients' quality of life.
Because most meats are high in phosphorus, the limiting factor in dietary phosphorus restriction in commercial diets is often the animal protein content. Determine the degree of protein reduction needed based on a patient's laboratory results and balance protein intake with adequate phosphorus restriction. Reduce protein, when appropriate, by maximizing protein quality to meet physiologic requirements without providing excess that contributes to uremic toxin production.
In contrast to patients with CKD without proteinuria, animals with marked protein-losing nephropathy (with or without concurrent tubular disease) may require as much or more attention to protein reduction as to phosphorus restriction to slow disease progression In many species, increasing dietary protein exacerbates glomerular protein loss. Albumin is toxic to renal tubules, leading to accelerated degradation of the entire kidney. So although it seems counterintuitive, most animals with protein-losing nephropathy respond to reduced dietary protein with lower urine protein:creatinine ratios (UPC) and higher serum albumin concentrations.
Unfortunately, no dose-response data exists to guide the amount of dietary protein that patients with renal disease should receive. For most patients with proteinuria, it is likely appropriate to feed a commercial renal diet, even if azotemia is not present. For dogs or cats consuming high protein/phosphorus diets (such as many grain-free and low-carbohydrate diets, raw diets or numerous meat-based treats) at diagnosis, reducing protein and phosphorus to near AAFCO minimum requirements may be a good initial step. Further dietary modifications can be based on laboratory results and clinical response.
Sodium
The vast majority of commercial pet foods contain sodium in excess of physiologic requirements. Because of primarily theoretical concerns about blood pressure and water balance, excess sodium is generally avoided in diets for patients with renal disease. The sodium content in all commercial renal diets for dogs and cats is above AAFCO minimum requirements, but less than the sodium content of most OTC diets.
Potassium
Serum potassium concentrations in animals with renal disease can vary dramatically among patients and between dogs and cats. Dogs with CKD are more likely to have hyperkalemia, especially those receiving ACE inhibitors for glomerular disease, while cats with CKD are more likely to have hypokalemia. Commercial renal diets also vary in potassium content, with feline diets generally containing more than canine diets. The wide range of potassium content in canine diets allows you to select a diet most appropriate for an individual patient. For dogs that have hyperkalemia while receiving a commercial renal diet that contains the lowest potassium content, a home-cooked diet may be an option if medications cannot be altered.
Acid-base
The kidney regulates acid-base balance through hydrogen ion excretion and bicarbonate regeneration; consequently, animals with renal impairment often become acidemic. Thus commercial renal diets are designed to be relatively alkalinizing. In cats, OTC maintenance diets are generally acidifying due to ingredient composition and because they are formulated to help prevent struvite-related urinary problems, so this feature makes them not ideal for cats with kidney disease, in addition to excessive phosphorus and/or protein and sodium.
B vitamins
B vitamins are water-soluble and with rare exception (i.e., vitamin B12) are not stored in the body. They are, however, needed daily for nearly all metabolic pathways. Most commercial renal diets for dogs and cats are fortified with additional B vitamins because of the potential for increased renal losses secondary to polyuria, although there are no data to support a benefit (or detriment) of supplementation at this time.
Omega-3 fatty acids
Research in dogs shows potential renoprotective effects of supplementation with long-chain omega-3 fatty acids from fish oil (eicosapentaenoic acid [EPA] and docosahexaenoic acid [DHA]). However, conflicting evidence exists, and a clear dose response has not been determined for dogs. Prospective studies on omega-3 fatty acid supplementation in cats with renal disease have not been published. Flax, a good source of the short chain omega-3 fatty acid alpha-linoleic acid (ALA), has not been investigated. As its endogenous conversion to DHA and EPA is poor in dogs and essentially nonexistent in cats, it should be used only as a last resort when fish oil supplementation is not feasible.
Many commercial renal diets contain varied amounts of added fish oil. With my patients, I use a total dose (DHA plus EPA) of about 300 mg per 10 lb body weight. This amount can be given with a commercial diet that does not already contain a supplement (taking into account the extra calories it provides), or you can calculate the total intake amount from the diet alone and add fish oil to obtain the desired dose. For many patients, liquid fish oil may also enhance palatability.
When should a renal diet be started?
In the absence of proteinuria, initial dietary modifications for early asymptomatic CKD (IRIS CKD stage 1 or when CKD is suspected but not confirmed) should be geared toward reducing phosphorus. A handful of OTC and veterinary therapeutic diets not necessarily intended for renal disease that contain phosphorus below 1.5 g/1000 kcal and a moderate amount of protein can be considered. These diets have higher protein content than do renal diets and may not otherwise be modified as discussed above . Once CKD progresses to IRIS CKD stage 3, or if proteinuria is evident, most patients should be fed only a commercial renal diet.
What about concurrent diseases?
Recently, new dry diets from Royal Canin have been introduced that combine hydrolyzed soy with low phosphorus and protein, which may be good options for dogs and cats with food allergies and kidney disease. Some patients with early CKD and confirmed or suspected food allergies or intolerances may be fed a commercial lower protein and phosphorus limited-antigen diet. Alternatively, a few of the regular renal diets can be fed on a trial basis to see if they are tolerated. For confirmed allergies to ingredients that cannot be avoided in the renal diets or for fat intolerance, home-cooked diet formulations may be required.
For pets with other health concerns, it is important to prioritize the diseases and their response to dietary management. For example, a dog with stage 2 kidney disease but severe chronic pancreatitis may be better off with a diet that has a bit more phosphorus but lower fat, at least until the kidney disease progresses further, at which time a home-cooked diet will likely be needed to manage both diseases.
A cat with stage 3 kidney disease and diabetes can be fed the lowest carbohydrate renal diet that it will eat and the insulin dose can be adjusted accordingly.
What if the pet will not eat a renal diet?
More than a dozen reduced-phosphorus and -protein renal diets (canned and dry) may be options for dogs with various stages of CKD. A slow diet transition is recommended when possible, and low-protein palatability enhancers such as fish oil, homemade low-sodium meat broths, honey, pancake syrup, applesauce and some human enteral nutrition products (for example Ensure Vanilla Nutrition Shake, which is low in both phosphorus and protein) can be added. Avoid meats and other foods high in protein, phosphorus and sodium as they may negate the benefits of the renal diet and make patients feel worse in the short term. Pets with later stage CKD commonly exhibit cyclical appetites and may not be interested in eating the same food every day. Rotating among several appropriate diets may help overcome this issue. Appetite stimulants such as mirtazapine rarely result in consistent consumption of enough food to meet energy requirements in patients with renal disease over the long-term.
Home-cooked diets may be more palatable to dogs with CKD than commercial diets. However, the vast majority of the recipes in books and online are unbalanced and may not be appropriate for renal patients despite assertions to the contrary.4 Clients wishing to try a home-cooked diet should obtain a custom recipe from a board-certified veterinary nutritionist, usually through a veterinary teaching hospital nutrition service. Veterinarians can also obtain balanced (but not customized) recipes for home-cooked renal diets for clients' pets from BalanceIT.com.
More than a dozen commercial canned and dry diet options for cats with various stages of renal disease exist. Cats tend to be notoriously picky about switching foods and transitioning them to a renal diet can be challenging. However, the potential to double their survival time and improve their quality of life should serve as powerful motivators to clients to persevere.
Cats also seem more likely than dogs to go through a prolonged period of wasting as their appetite decreases and their intake does not meet their energy requirements. Unlike in dogs, appropriate home-cooked diets are rarely more appealing to cats than commercial diets. Use palatability enhancers such as homemade low-sodium meat broths, fish oil and animal fats to encourage intake. CliniCare RF Feline Liquid Diet may be palatable to some cats and can supplement their food consumption.
Assisted feeding
Consider assisted feeding for patients with renal disease that do not voluntarily consume sufficient calories of an appropriate diet for their disease to maintain appropriate body condition. Esophagostomy tubes are most commonly used because a blenderized canned renal diet can be given in adequate amounts, along with certain medications and oral fluids. This reduces the stress associated with mealtimes and helps enhance quality of life for pets and owners.
It's best to place a feeding tube before a patient is severely debilitated and not as a last-resort attempt to prolong life in an emaciated, anorexic, severely uremic animal. I often discuss feeding tubes with clients at the first or second visit after renal disease is diagnosed, and advise them that a feeding tube may be needed in the future and to decide as a family how to handle the situation. In my experience, clients make better emotional decisions when their pet is not in immediate danger and they have ample time to consider a course of treatment. Also consider keeping a list of clients who've successfully used feeding tubes for their pets and are willing to share their experiences with other clients.
References
1. Ross SJ, Osborne CA, Kirk CA, et al. Clinical evaluation of dietary modification for treatment of spontaneous chronic kidney disease in cats. J Am Vet Med Assoc 2006;229:949-957.
2. Jacob F, Polzin DJ, Osborne CA, et al. Clinical evaluation of dietary modification for treatment of spontaneous chronic renal failure in dogs. J Am Vet Med Assoc 2002;220:1163-1170.
3. Cortadellas O, Fernandez del Palacio MJ, Talavera J, et al. Calcium and phosphorus homeostasis in dogs with spontaneous chronic kidney disease at different stages of severity. J Vet Intern Med 2010;24:73-79.
4. Larsen JA, Parks EM, Heinze CR, et al. Evaluation of recipes for home-prepared diets for dogs and cats with chronic kidney disease. J Am Vet Med Assoc 2012;240:532-538.
Dr. Cailin Heinze is associate professor of nutrition at Cummings Veterinary Medical Center at Tufts University in North Grafton, Massachusetts.