kidney failure pancreatitis dog
Pancreatitis in Dogs Symptoms, Causes & Treatment
Pancreatitis in dogs is one of those conditions that owners must be informed about before it strikes because the warning signs may not always be obvious at first, the symptoms might be mistaken for something less serious, and yet its potentially life-threatening. The medical definition of pancreatitis is simple: inflammation of the pancreas. But like all serious conditions, there is more to it than that.
Because it is dangerous, a suspected case of pancreatitis needs to be addressed by a veterinarian as quickly as possible and not dealt with by DIY treatments. As with all medical issues, even the best online resource is not a replacement for the medical guidance from your vet.
Before looking at the details of pancreatitis, lets take away the ititis and explain the small but vital organ itself:
The pancreas is responsible for releasing enzymes that aid in digestion. When the organ is working normally, the enzymes become active only when they reach the small intestine. In a dog with pancreatitis, however, the enzymes activate when theyre released, inflaming and causing damage to the pancreas and its surrounding tissue and other organs. According to the Whole Dog Journal, the enzymes can actually begin to digest the pancreas itself, which causes extreme pain to your dog.


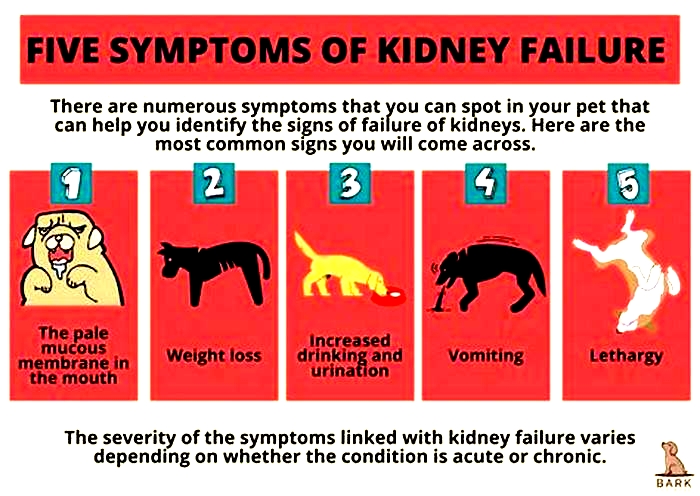
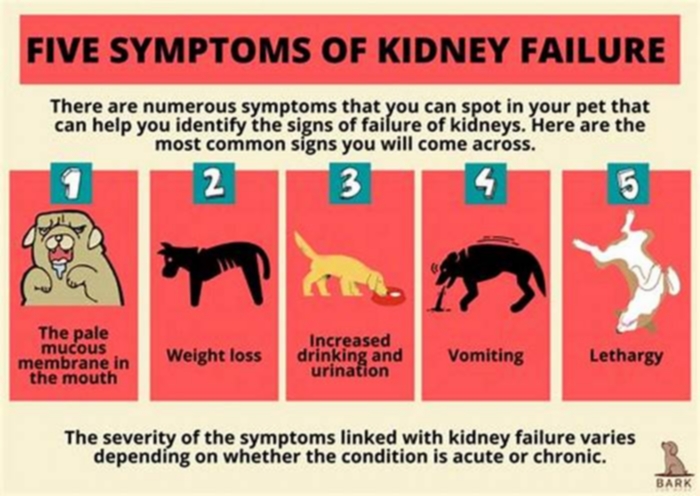
Classic signs of pancreatitis in dogs
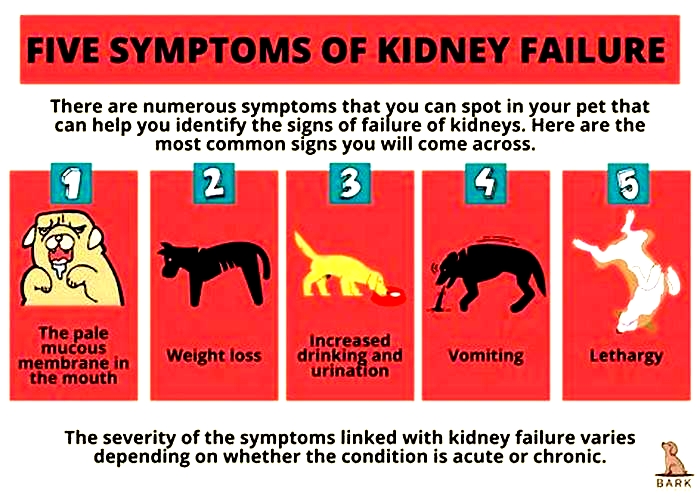
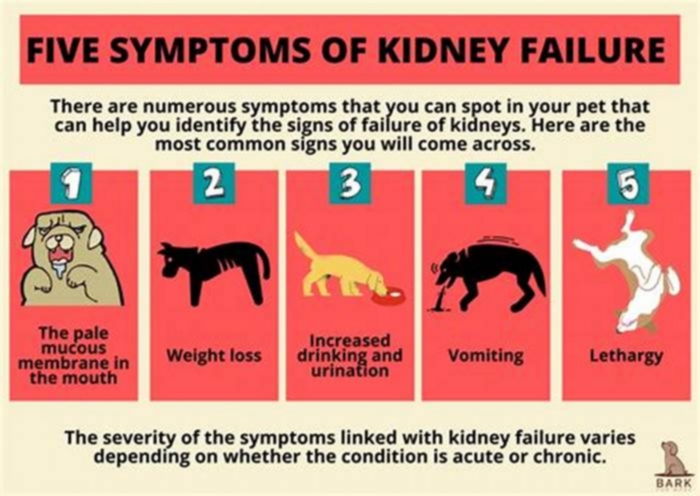
- Hunched back
- Repeated vomiting(either several times within a few hours or periodically over several days)
- Pain or distention of the abdomen (dog appears uncomfortable or bloated)
- Diarrhea
- Loss of appetite
- Dehydration
- Weakness/lethargy
- Fever
If your dog exhibits one of these signs, and only infrequently, monitor her. But if she exhibits multiple signs at once, and repeatedly, a call to the veterinarian quickly is vital.
Dehydration and pancreatitis in dogs
Dehydration is due to a greater fluid loss than fluid intake. Diarrhea or vomiting can cause dehydration, but those signs together will cause a greater fluid deficit and dehydration because the dogs fluid input (drinking) cannot keep up with the fluid losses. If the diarrhea becomes bloody, the condition worsens and the dehydration can become an emergency.
Other factors such as fever require increase fluid intake and can lead to dehydration along with other metabolic issues such as kidney disease, etc.
Blood in a dogs stool indicates a loos and significant inflammatory response requiring a veterinarians attention but it can be cause by a multitude of factors, from ulceration to parasites. Dehydration is a serious condition that can lead to death. It is an emergency and requires immediate veterinary care.
Any lethargic dog who is not drinking water or cannot hold water down should be suspect of dehydration and examined by a veterinarian. Dry mucous membranes (such as gums) may be a quick way of assessing dehydration but as always, when in doubt, consult with your veterinarian.
Causes of pancreatitis in dogs
There are a number of causes and risk factors that can bring on pancreatitis. Though often the attack appears seemingly out of the blue. Among them are:
- A high-fat dietThis is a major cause of pancreatitis, especially for a dog who gets one large helping of fatty food in one sitting
- A history of dietary indiscretion (a medical term for saying your dog will eat anything)
- Obesity
- Hypothyroidism (or other endocrine diseases)
- Severe blunt trauma
- Diabetes mellitus
- Certain medications or other toxinsThese include cholinesterase inhibitors, calcium, potassium bromide, phenobarbital, l-asparaginase, estrogen, salicylates, azathioprine, thiazide diuretics, and vinca alkaloids.
- There may, in some cases, be a genetic predisposition. Certain breeds or types of dogs have been associated with higher risks of pancreatitis such as Miniature Schnauzers and some of the smaller toy and terrier breeds.
More about those fats: Human food is especially dangerous, though even high-fat dog food may cause pancreatitis. So owner vigilance is particularly required around holidays and other festive occasionsthey can bring well-meaning guests who slip your buddy a fatty piece of lamb, or a tray of buttery cookies left within reach of an eager muzzle. In fact, the day after Thanksgiving is known for more than just Black Friday bargains. Its one of the busiest days of the year pancreatitis-related emergency vet visits.
Basically, if your dog is showing any signs of abdominal pain, the worst thing to do is feed him a fatty diet. This is one of many reasons that giving your dog table scraps, as tempting as it may be, is not advisable.
How does a vet diagnose pancreatitis in dogs?
- Your dogs medical history
- Blood tests to measure pancreatic enzymes
- Physical examination including stomach, gums, heart, temperature
- Radiographs or ultrasound, to rule out other causes
- Fine needle aspiration of the pancreas
As the Merck Veterinary Manual notes, as with any disease, no test should be used in isolation for diagnosis, and all clinical findings should be used in conjunction to arrive at the most appropriate diagnosis.


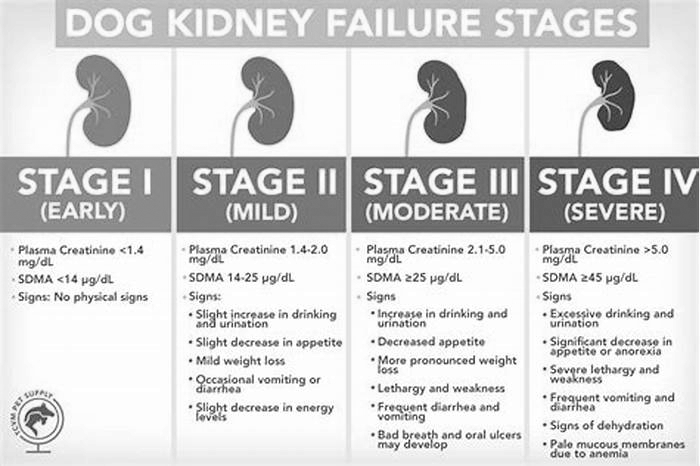
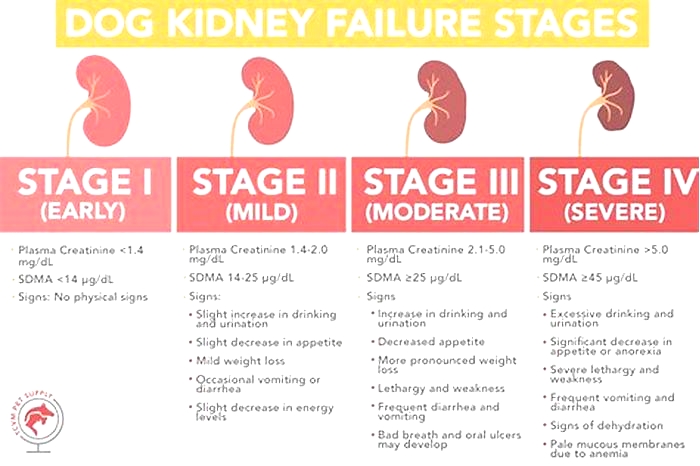
Whats the difference between acute and chronic pancreatitis?
Acute PancreatitisAn acute attack of pancreatitis means it comes on suddenly, with no previous appearance of the condition before. It can become life threatening to other organs if the inflammation spreads.
Chronic PancreatitisA chronic condition is one that has developed over time, slowly, and often without symptoms. This condition can result from repeated bouts of acute pancreatitis.
Both acute and chronic forms can be either severe or mild, and both result in pain.
Treatment and management of pancreatitis in dogs
Theres no fancy treatment for acute pancreatitis. First and foremost, your dogs pain must be managed, and early intervention to prevent further complications is key. The most common treatment and management options are:
- Intravenous (IV) fluid therapy in severe pancreatitis
- Vigorous monitoring of a worsening condition
- Antiemetic medication for vomiting (to prevent dehydration)
- Resting the pancreas (withholding food and water for 24 hours)Long-term management includes:
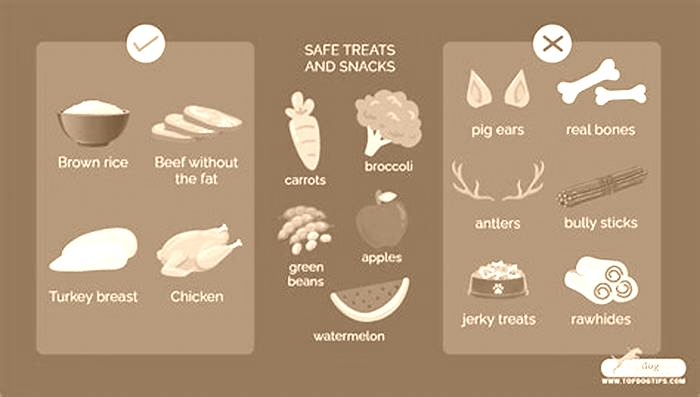
- Vigilant monitoring of fat intakeNo table scraps allowed!
- Use of a prescription diet of gastrointestinal-supportive low-fat, or ultra-low fat, food.
- Feed smaller, more frequent meals instead of one larger meal
- Have amylase and lipase levels checked by a veterinarian regularly
Can supplements be used to prevent or manage pancreatitis in dogs?
It is important to reiterate that pancreatitis is a serious condition, so home remedies shouldnt be used in place of veterinary intervention. That said, some vets believe digestive enzyme supplements with pancreatin can help some (not all) dogs by reducing the work of the pancreas and inhibiting pancreatic secretion. These come in over-the-counter strength as well as prescription strength.
Fish oil may seem counterintuitive at first, because of its high fat content, but it can actually help lower blood lipid levels. Studies suggest a high level of fish oil (about 1,000 mg. per 10 pounds of body weight for dog with high lipid levels; about half that amount for dogs with normal levels) is helpful to dogs with acute pancreatitis. When supplementing with fish oil, also supplement with 5 to 10 IU of vitamin E.
There have been human studies suggesting that vitamin E (with selenium), vitamin C, beta-carotene, and methionine may help prevent pancreatitis. Conversely, another human study reveals that probiotics can make acute pancreatitis worse.
Always speak with your veterinarian before offering any supplements to your pet.


A canine researchers case study: her own dog
Caroline Coile, Ph.D is the Nutrition and Health columnist for AKC Family Dog and a two-time AKC Canine Health Foundation Award winner. Pancreatitis is a subject Coile knows well, not only as a professional canine researcher and writer, but because her dog, a Saluki named Beanie, went through the difficult and stressful experience. Here she shares her story:
Beanie, unlike most Salukis, loves to eat. But one day, after eating his very favorite treata flaky biscuithe vomited it up. He was standing with his back kind of hunched. I gently pressed on his abdomen, and he yelped. Out came the thermometer, which told me his temperature was 103 degrees. While I was calling the veterinarian, he vomited again, then lay down in a corner. We were in the car within minutes.
The veterinarian palpated his abdomen, which was definitely tender; took his temperature, which was still high; and drew blood. Beanie received pain medication, antibiotics, and intravenous fluids to combat fluid loss and came home with strict instructions not to eat that day. Eating anythingor even smelling foodcould have caused his pancreas to secrete enzymes and slow its healing. He could lick ice cubes, and then drink a bit of water.
The next day, he was allowed to eat about six tiny meals of low-fat, high-carbohydrate food. This meant rice, potatoes, or pasta. Overcooking these starchy foods makes them easier to digest. We would boil one cup of white rice (not instant rice) in four cups of water for 30 minutes to make a rice porridge called congee. We gradually added in protein sources, such as skinless chicken breast, low-fat cottage cheese, or boiled hamburger meat. When feeding a dog with pancreatitis, its important to cook all the food even if you normally feed a raw diet. Because the dogs gut is compromised, its necessary to remove fat and destroy bacteria.
After a week, Beanie progressed to a veterinary prescription diet for dogs with pancreatitis. He hated it. Many dogs with a history of acute pancreatitis must be on a special diet for the rest of their lives. If they dont like the pancreatitis diet, a low-fat weight loss diet often works just as well. Since obese dogs are more prone to pancreatitis, they need to lose weight anyway. Even if a high-fat meal didnt cause the initial bout, it can trigger a recurrence once the dog has had pancreatitis.
After a month, Beanie was able to gradually transition back to his old diet, minus the high-fat treats. Eventually, he even got his breakfast biscuitsbut no more butter. He never had another bout of pancreatitis.
The Take-Away
As the Canine Journal puts it, pancreatitis is like that relative that just wont leave: Even when theyre gone, the thought of their return hovers in the back of your mind. Unfortunately, once a dog has had a bout of pancreatitis, the chance of recurrence is high. You best defense against a repeat appearance of this unwelcome intruder is a two-pronged approach: Be on the look-out for the warning signs and control the things you can. Dont let your dog become obese (exercise is good for both of you), follow your vets feeding instructions strictly, and, when relevant, administer your dogs medication faithfully.
Mild cases of pancreatitis usually have a good prognosis. Severe cases have a more guarded prognosis, due to the potential for systemic complications. But as a vigilant, responsible, and most of all, knowledgeable dog owner, you now know what you can do to reduce the risk of pancreatitis, how to recognize it if it does strike, and how to manage it going forward.
Pancreatitis in Dogs and Cats
Chronic cases: as above, with monitoring of progression, and, if there is no improvement, trial therapy with an immunosuppressive agent
The mainstay of therapy of severe pancreatitis is supportive care with fluid therapy, vigorous monitoring, and early intervention to prevent systemic complications. Fluid therapy should be based on calculation of degree of dehydration (to be replaced over 48 hours if there is no contraindication), maintenance, and ongoing losses (eg, due to vomiting or diarrhea).
In those few cases in which the cause is known, specific therapy against the inciting cause may be initiated. Antibiotics are of questionable value and should not be used routinely.
Resting the pancreas is suggested only if the animal vomits uncontrollably (ie, the animal vomits frequently and violently despite appropriate antiemetic therapy). In fact, early nutritional support is considered a key component of successful treatment of human patients with severe pancreatitis. Also, enteral nutritional support is considered superior to parenteral nutrition. Animals that vomit should be treated with an antiemetic, such as maropitant (NK1 antagonist), ondansetron, or dolasetron (HT3 antagonists), or in most animals a combination of both. Even animals that do not actively vomit may benefit from such antiemetic support, because they may be nauseated, leading to poor or absent appetite. Metoclopramide is not considered effective as an antiemetic agent and should not be used in these animals.
Abdominal pain should be assumed to be present and treated until contrary evidence is available. Intermittent meperidine, butorphanol, or buprenorphine may be used in animals with mild or moderate abdominal pain. Animals with severe pain are often treated with a constant-rate infusion of an opioid, such as morphine, fentanyl, or methadone, or with a combination therapy of fentanyl, ketamine, and lidocaine. Many other treatments have been investigated in dogs, cats, and people, but unfortunately none has been shown to be useful.
Recently, a new medication for the specific treatment of acute pancreatitis, Brenda Z, an LFA-1 antagonist, has been licensed for the treatment of acute canine pancreatitis in Japan. Although initial reports are very promising, this medication has not yet been licensed for use in either North America or Europe.
Animals with mild forms of pancreatitis should be carefully assessed for the presence of risk factors (eg, hypertriglyceridemia, hypercalcemia, history of medications that can cause pancreatitis) and concurrent diseases (eg, cholangitis, hepatitis, inflammatory bowel disease, diabetes mellitus). In dogs, feeding an ultra-low-fat diet is crucial for treatment success. In cats, a moderately fat-restricted diet is recommended. Antiemetic drugs (see above) and appetite stimulants (ie, capromorelin in dogs, mirtazapine in cats) are helpful for animals that may not eat due to nausea.
If animals with chronic pancreatitis do not respond to therapy, a trial with prednisone (dogs), prednisolone (dogs and cats), or cyclosporine (dogs or cats) may be attempted. Cyclosporine is advantageous in animals with concurrent diabetes mellitus, because it has a smaller impact on insulin resistance than glucocorticoids.
The prognosis in mild cases of pancreatitis is good, but the prognosis in severe cases of pancreatitis is guarded in both dogs and cats. Systemic complications such as hypothermia, acidosis, hypocalcemia, and single- or multiple-organ failure are considered risk factors for a poor outcome. It can be challenging to identify severe cases early during the disease process and prevent complications in those animals.