kidney disease dogs bun levels
Watch Out for a Misdiagnosis of Chronic Kidney Disease in Dogs
This is a quiz. When a laboratory test performed on your dogs blood shows elevated blood urea nitrogen (BUN) and creatinine levels that indicate kidney problems, the most likely cause is:
A) chronic renal failure (CRF)B) a bacterial infectionC) a tick-borne diseaseD) an endocrine imbalanceE)a urinary tract infection
If you guessed A, youre not alone. For many conventional veterinarians, this ones a no-brainer. When BUN and creatinine levels are higher than normal, many American vets assume the cause is chronic renal failure (CRF), and often all they prescribe is a low-protein dog food (see When to Say No to Low Protein).
But the patient may not have chronic renal failure at all. Instead, a bacterial infection like leptospirosis, a tick-borne disease like ehrlichiosis, an endocrine imbalance like Addisons or Cushings disease, or a urinary tract infection may cause the elevated readings.
If thats the case, time is of the essence. Your dog may need medical treatment RIGHT NOW, and every moment you lose to a misdiagnosis can cost him his life.
Dogs that suddenly go into kidney failure may have an acute disease that is curable, says San Francisco Bay Area canine health researcher Mary Straus. I hear over and over again about dogs being diagnosed with chronic kidney failure and given nothing but a bag of k/d to take home when in fact they had a serious but treatable illness that caused elevated kidney values. If these dogs had been diagnosed early enough, their veterinarians could have given them appropriate treatment, and their lives might have been saved.
Acute Renal Failure in Dogs
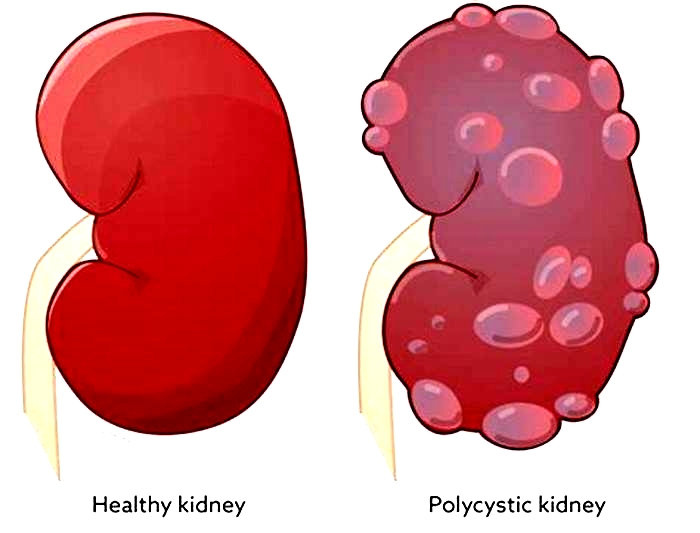
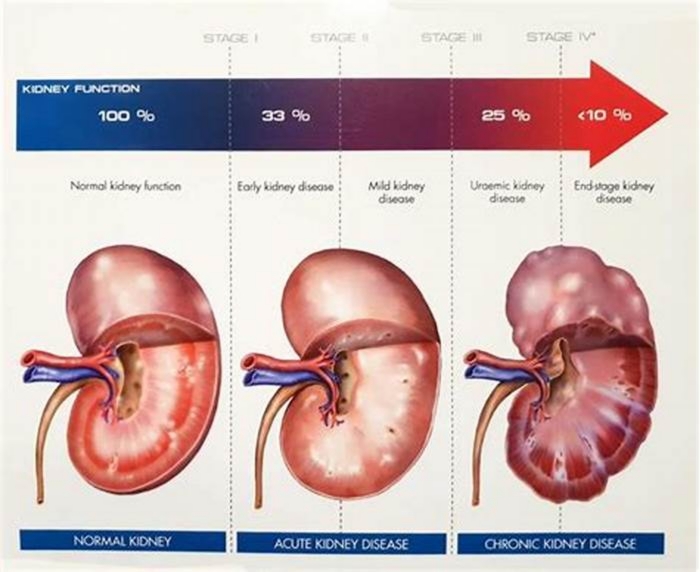
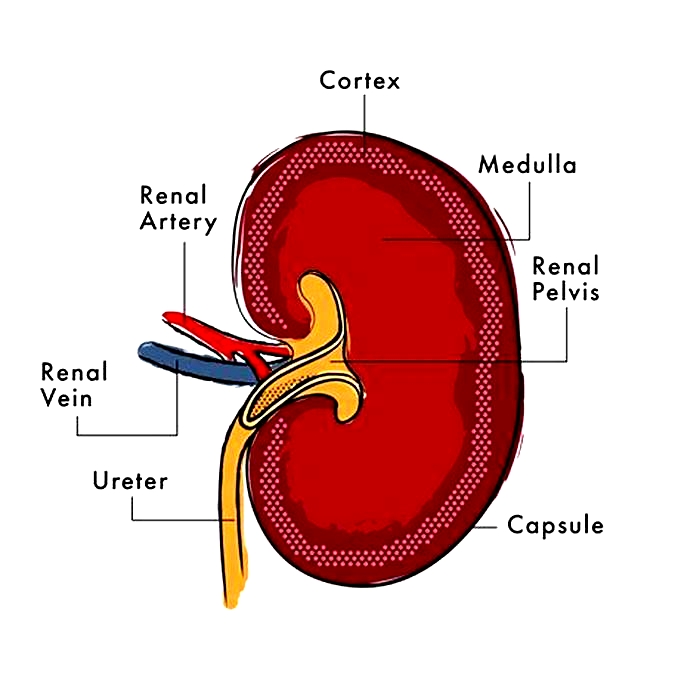
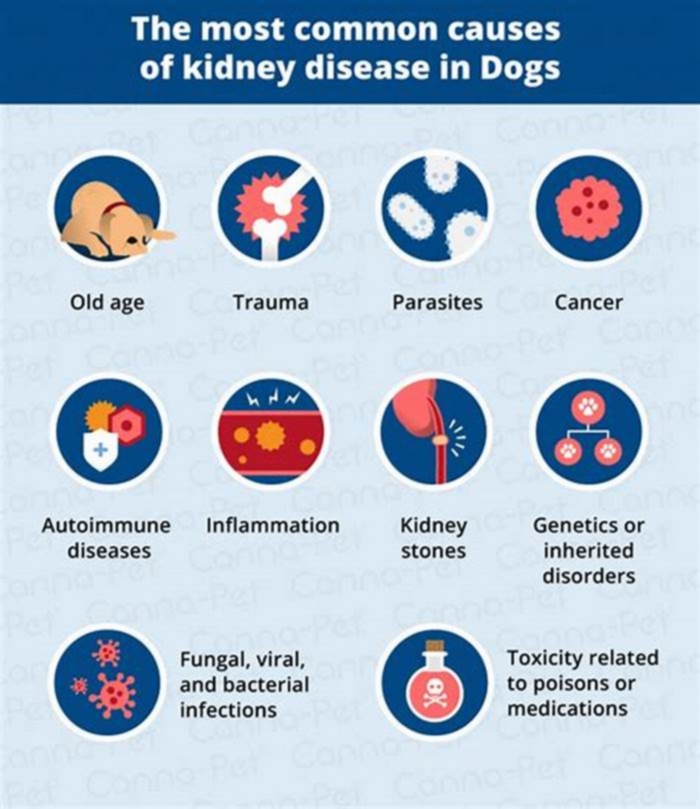
Unlike chronic renal failure, which is a progressive illness that can take years to develop, acute renal failure is a crisis involving the sudden loss of kidney function. It can be caused by a number of health disorders, such as infection, toxins or chemicals (including many medications), and any illness that damages the kidneys or interferes with kidney function.
The most common cause of acute renal failure is exposure to a toxin, such as antifreeze, rat poison, certain antibiotics, heavy metals, nonsteroidal anti-inflammatory drugs (NSAIDs), or ingesting large amounts of grapes or raisins.
Be sure to report any such exposure, or the possibility of exposure, to your veterinarian. The fast and accurate identification of a toxin your dog ingested can make the difference between life and death. It is also important to consider all drugs that your dog is currently taking, and check the package inserts to see if renal failure is a possible side effect. Some dogs on NSAIDs develop symptoms of kidney failure without their vets realizing that the drugs should be stopped, says Straus.
Bacterial infection, such as from leptospirosis, can also cause acute renal failure. This type of infection will not show up on a urinalysis or urine culture. But its still a good idea to do a urinalysis and culture for all dogs with elevated creatinine and BUN levels, says Straus.
Urinary tract infection can cause elevated kidney values if the infection ascends into the kidneys, she says. Infections are also common in dogs with chronic renal failure. A urine culture should be done to rule out infection, as approximately 20 percent of urinary tract infections will not show up on a urinalysis alone.
Any time a dog, especially one thats young or middle-aged, becomes acutely ill or suddenly develops signs of kidney failure, you have to look for the cause. It can be something the dog may have gotten into, a drug hes taking, a simple infection, or an unsuspected illness. It probably isnt chronic renal failure, as the symptoms of that disease develop slowly.
When Leptospirosis Looks Like Kidney Failure
In the fall of 2003, Texas resident Lew Olsons 15-month-old Rottweiler, Bean, became listless, lost his appetite, urinated often, and had a constant craving for water.
I took him for routine tests, which included a complete blood panel and urinalysis, Olson says. Because Bean already had kidney problems, as soon as the tests showed that his kidney values were suddenly quite high, our veterinarian assumed that he would soon die from chronic renal failure and that nothing could be done to save him.
Luckily for Bean, Olson refused to accept this diagnosis. While she searched frantically for answers, Bean began to dehydrate. He lay curled in a ball and had a slight fever. Thats when we started IV fluid therapy, she says. We also ran a series of lab tests that included a tick disease panel and fungal panels. All came back negative.
Olson searched the Internet for any illness she could find that matched her dogs symptoms. One thing started popping up over and over, and that was leptospirosis. However, all the sites I found talked about elevated liver enzymes, which did not show up on Beans blood panel results.
Then eight-year-old Striker, another of her 16 Rottweilers, became sick with the same symptoms. I went back to researching leptospirosis and found that there are nine different strains, two of which do not affect the liver but have a delayed reaction in attacking the kidneys.
Olson quickly asked for blood titer tests for leptospirosis. The test takes several days, she says, so we went ahead and started both dogs on penicillin, which is the treatment of choice for lepto. We also continued the IV therapy, as keeping an affected dog hydrated is paramount in treatment.
Both Bean and Striker tested positive for leptospirosis. My veterinarian was shocked, Olson says, but I was relieved to know that we now had a diagnosis and a protocol for treatment.
Olson posted her dogs story online to help others understand leptospirosis. Most veterinarians are familiar with the two most common forms of this disease, she explains, but the newer strains are often missed and simply seen as CRF.
Olson receives e-mail messages every week from people whose dogs are diagnosed with CRF but show symptoms suggesting leptospirosis. At least 50 percent of these dogs test positive for lepto, she says, and many are saved. Lepto is becoming an epidemic, but few veterinarians recognize it or call it anything other than CRF. I know of cases in almost every part of the United States and some in Canada. Its a shame because of all the illnesses that are confused with chronic renal failure, lepto is the easiest to treat if its caught in time.
Leptospirosis is spread by squirrels, rats, and other wild and domestic animals, usually through contact with infected urine. One strain, Leptospira canicola, used to be called lamp-post disease because city dogs, especially males, were said to infect themselves by sniffing around lamp posts soaked with the urine of infected dogs.
Dogs can also be exposed by drinking stagnant water containing infected urine or through close contact with an infected animal. Males, because of their personal habits, and dogs with immune system disorders are most at risk. Surprisingly, younger dogs are more likely to be infected than older dogs, though dogs of all ages and either sex can get the disease.
Leptospirosis is most common in the spring and fall or any rainy season. Leptospira bacteria cannot survive when temperatures are below freezing or above about 80oF. The incubation period is 4 to 12 days.
Symptoms vary depending on the infected animals age and condition as well as the strain involved. Leptospirosis can generate fever, dehydration, loss of appetite, vomiting, thirst, rapid weight loss, fetid breath, red eyes, tenderness or pain in the abdomen or joints, lack of energy, and depression. Some strains produce elevated liver enzymes and possibly symptoms of jaundice. Progressive kidney failure accompanies the infection, but kidney function can return to normal soon after recovery. Severe leptospiremia produces fevers up to 104o to 105o F, shivering, shock, and death.
Because the leptospirosis titer test is time-consuming and may not be accurate, especially during initial infection, most experts recommend immediately treating the disease based on its symptoms and verifying the diagnosis when results are available. Most dogs show some but not all of the symptoms listed above. Some show only increased drinking and urination, combined with low urine specific gravity. Because leptospirosis is far more common than most people and vets realize, whenever symptoms of kidney disease develop suddenly, presumptive treatment for lepto may be a good idea.

Treatment includes intravenous fluids to prevent dehydration and keep the kidneys functioning well. Both of Lew Olsons dogs were on IV therapy for five to seven days. Penicillin is generally recommended for three weeks, followed by two to three weeks of doxycycline, an antibiotic that stops infecting bacteria from being shed and transmitted in the dogs urine.
Leptospirosis vaccines are available, but they do not cover all strains, and protection only lasts a few months. Even recently vaccinated dogs can become infected with leptospirosis.
Ehrlichiosis Can Look Like Kidney Failure
Last winter in Washington, DC, Amy Malls four-year-old mixed breed, Louie, started showing minor symptoms.
One was that he needed to go out a little earlier in the morning, Mall recalls. I completely ignored this. Then he started getting very picky about food. This was a 75-pound powerhouse who ate everything in sight. I called my vet and said he was acting finicky, and she said to just keep trying new things, and if he wouldnt eat anything at all to bring him in.
One morning I saw him shivering, and I took him to the vet straight away. She did blood tests and called me to say his kidneys were failing. She sold me a bag of k/d dog food and said there was nothing else to do for him. Luckily, she also said that if I really wanted to, I could go see a specialist.
The next day, the specialist put Louie on antibiotics and tested him for possible illnesses. The test for ehrlichia, a tick-borne infection, came back positive.
I wish the first vet had known that picky eating was a possible symptom, says Mall, or asked me if I had noticed any other changes, like his needing to go out earlier in the morning. I kick myself for not being more assertive, but I just didnt know. Im lucky to have access to a specialist, but I think most of my vets clients would have just taken the k/d and watched their dogs die. Unfortunately, my dog died, too, as I did not catch the ehrlichia early enough.
Courtney Alieksaites of Dallas, Texas, was more fortunate. Last November, her Miniature Dachshund puppy, Napoleon, developed a high fever and was hunched over in pain. He was diagnosed with a fever of unknown origin, treated with antibiotics, and kept on intravenous fluids for three days, she says. Finally, the fever broke, and he got better.
In February, the same symptoms returned, though less severely. When Napoleon arrived at the clinic, a new veterinarian reviewed his chart and on the basis of previous blood tests prescribed a low-protein food.

I was trying to make sense of this, says Alieksaites, so I went online and started asking questions. When I described Napoleons symptoms, several people suggested that we have him tested for ehrlichia. The test came back positive. Im so glad I persevered and looked for answers that went beyond chronic renal failure and k/d dog food. We go to a different clinic now, and since Napoleon was treated for ehrlichia, hes been back to his favorite activities, which are eating all his favorite foods and snuggling on my pillow.
Of the diseases transmitted by tick bites, ehrlichiosis is the most likely to be confused with chronic renal failure. It is caused by Ehrlichia, a member of the rickettsiaceae family of organisms similar to bacteria. Dogs can become infected with several species of Ehrlichia, but E. canis is the most common and causes the most severe illness.
The disease was not well understood until ehrlichiosis infected hundreds of military dogs returning from Vietnam, giving it the names tracker dog disease and tropical canine pancytopenia. German Shepherd Dogs and Doberman Pinschers seem particularly vulnerable. Dogs testing positive for E. canis have been identified throughout the U.S., with most concentrated where the brown dog tick is common, such as in the Southwest and along the Gulf coast.
Eight to 20 days after a bite from an infecting tick, a dog experiences the acute phase of ehrlichiosis, which produces fever, swollen lymph nodes, breathing problems, weight loss, bleeding disorders, and in some cases, neurological disturbances. Symptoms can be obvious or so mild that they go unnoticed. This phase usually lasts two to four weeks.
In the subclinical phase of infection, the organism remains present without causing obvious symptoms. If their immune systems are strong enough, dogs may be able to keep the organism in check for months or years before stress, illness, or treatment with steroids weakens the immune system, allowing the infection to become active again. When that happens, dogs enter the chronic stage of infection.
Mild chronic ehrlichiosis causes weight loss and indistinct, elusive indications of illness. Severe chronic ehrlichiosis causes anemia, decreased platelets resulting in bleeding episodes, limping or lameness, eye hemorrhage, neurological problems, swollen legs, severe weight loss, and, eventually, bone marrow failure, an inability to manufacture the blood cells needed to sustain life.
Ehrlichiosis is difficult to diagnose in its earliest stages because antibody tests typically come back negative. It takes the immune system two to three weeks to respond and develop antibodies, which is why a diagnosis made soon after a tick bite cant be confirmed until the test is repeated weeks later. When tick disease is suspected, presumptive treatment to see if the dog improves can confirm that the treatment is appropriate.
Dogs experiencing severe anemia or bleeding problems may require a blood transfusion. Doxycycline is the drug of treatment, but another tetracycline drug may be used for dogs unable to tolerate doxycycline. Conservative treatment lasts for 10 to 30 days, but veterinarians working in the field prefer to treat with 5 mg doxycycline per pound of body weight every 12 hours for two months, as this protocol results in fewer recurrences of the disease.
It is very dangerous to give steroids to a dog with tick disease, says Mary Straus, because steroids suppress the immune system and make the dog more vulnerable to the infection. Steroids are sometimes used when immune mediated hemolytic anemia is present, but they must be given concurrently with antibiotics. If a dog develops symptoms of kidney disease following any treatment with corticosteroids, tick disease should be suspected.
Because tick-borne diseases imitate many illnesses, its a good idea to test for them whenever treatment for what seems to be the causative factor is ineffective.

It Might Be Addisons Disease
Two years ago, a three-year-old Nova Scotia Duck Tolling Retriever belonging to William Smith in California (names have been changed) showed elevated BUN on routine blood work.
Two months earlier, Duxs diet had been switched from commercial food to a home-prepared raw diet. Smith was told to reduce the diets protein levels, which he did, but Dux began to experience lethargy, loss of appetite, severe weight loss, and, eventually, vomiting. Repeat blood work showed even higher BUN, along with elevated phosphorus and potassium.
Dux was treated by three veterinarians, all of whom disapproved of his diet. The holistic vet said to add more vegetables to his food so that he wouldnt eat so much protein, says Smith. The conventional veterinarian didnt like the raw diet at all and blamed Duxs elevated BUN count on his new food. The third vet said to stay with conventional Western medicine until his condition stabilized.
But what was Duxs condition? Only after Smith pushed for a definite diagnosis and insisted on an ACTH Stimulation test, based on Duxs elevated potassium and low sodium/potassium ratio, did he learn that his dog had Addisons disease, not chronic renal failure.
In canine Addisons disease (hypo-adrenocorticism), the dogs adrenal glands produce too little cortisol. Its main symptoms include loss of appetite, weight loss, lack of energy, weakness, vomiting, diarrhea, and dehydration. Some cases involve blood in the stool or vomit, excessive thirst or urination, hair loss, and shaking or tremors. Most dogs show only some of these symptoms, which may come and go over time. Eventually, the dog may collapse in shock with what is called an Addisonian crisis, which is fatal without treatment.
An estimated 70 to 85 percent of dogs with canine Addisons Disease are female, and most are between four and seven years old. Great Danes, Labrador Retrievers, Nova Scotia Duck Tolling Retrievers, Portuguese Water Spaniels, Rottweilers, Standard Poodles, West Highland White Terriers, and Wheaten Terriers seem to be affected more than other breeds. However, dogs of either sex and of all breeds and ages can develop Addisons disease.
Addisons is treated with hormone medication that supplies what the adrenal glands can no longer produce.
When Cushings Disease Looks Like Kidney Failure
Canine Cushings disease, or hyperadrenocorticism, is often mistaken for the aging process because it usually occurs in older dogs who lose their hair, gain weight, urinate in the house, and seem to experience neurological changes.
Cushings disease is the opposite of Addisons, for here the body produces too much cortisol. The underlying cause is usually a pituitary or adrenal tumor, although veterinary treatment with steroid drugs can cause similar symptoms.
The average canine Cushings patient is 10 years old and spayed or neutered. While all breeds are at risk, Poodles, Beagles, Boston Terriers, Boxers, Cocker Spaniels, Dachshunds, German Shepherd Dogs, Golden Retrievers, Labrador Retrievers, Australian Shepherds, and small Terriers are most susceptible.
Increased or excessive water consumption and urination, urinary accidents in house-trained dogs, increased or excessive appetite, a sagging or bloated appearance, lethargy, hind-leg weakness, excessive panting, hair loss or a dull, dry coat, and easily damaged skin are a few of the most common symptoms. Treatment depends on the underlying cause of the illness as well as the patients overall health.
Elevated BUN Levels Might Not Be Anything At All
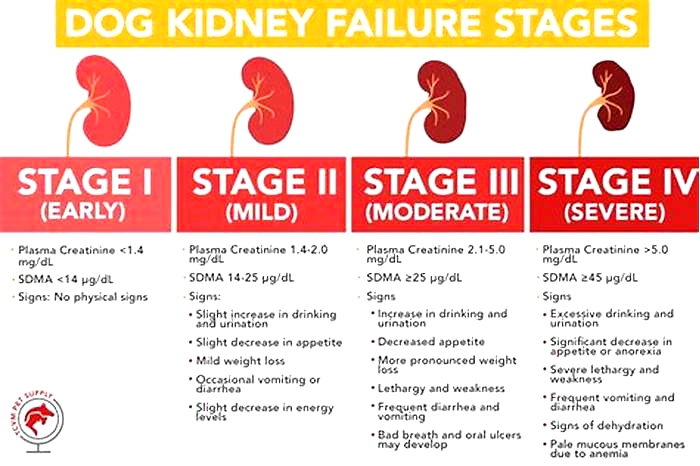
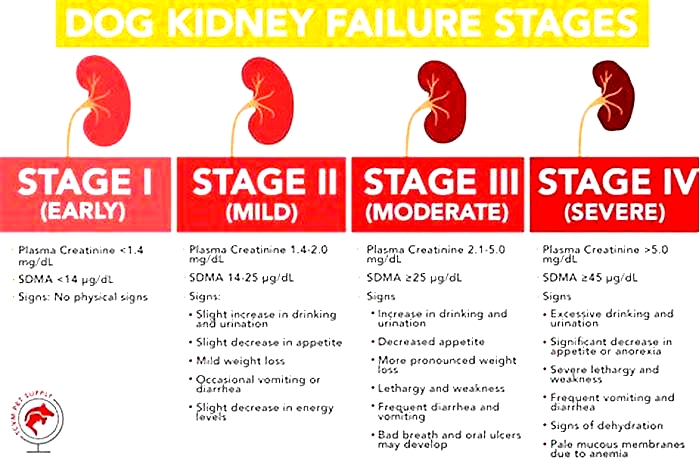
Some dogs are diagnosed with kidney disease based on nothing other than a slightly elevated BUN. Mildly elevated BUN can be caused by a recent meal or by minor dehydration. If your dogs creatinine and urine specific gravity are normal, your dog does not have kidney disease. It is best to do blood work after fasting your dog for at least 12 hours and to test urine specific gravity with the first catch of the day for accurate results.
Any unusual blood test results can be frightening, but knowledge is power. Learning about leptospirosis, ehrlichiosis, Addisons disease, Cushings disease, and urinary tract infections can help you notice and keep track of important symptoms, ask the right questions, request the right tests, avoid misdiagnosis, and obtain the right treatment to keep your best friend happy and healthy for years to come.
KIDNEY FAILURE IN DOGS: OVERVIEW
1. If your dog suddenly develops symptoms of kidney disease, look for the cause instead of assuming chronic renal failure.
2. Blood work abnormalities (in addition to elevated creatinine and/or BUN) may be clues. Discuss them with your vet.
3. Mention all of your dogs abnormal behavior and health to your vet; any clue might further a correct diagnosis.
4. Get a second opinion or see a specialist if needed.