dog kidney failure vomiting blood
When Dogs Vomit Blood Causes, Prevention, and Treatment

When Dogs Vomit Blood Causes, Prevention, and Treatment
Overview of Hematemesis (Vomiting Blood) in Dogs
Vomiting blood in dogs is one of 21 symptoms that should never be ignored.
The medical term for vomiting blood is hematemesis, which is the presence of flakes, streaks, or clots of fresh blood in the vomitus, or the presence of digested blood in the vomitus. Digested blood can be described as looking like coffee grounds. There are various causes for vomiting blood and the effects on the animal are also variable. Some are subtle and minor ailments, while others are severe or life threatening.
Hematemesis may be the only clinical sign, or it may be accompanied by other clinical signs. It can be difficult for the pet owner to distinguish between true hematemesis, which involves bleeding within the gastrointestinal tract, from secondary hematemesis, which involves the vomiting of swallowed blood. Sneezing or coughing blood, and/or blood dripping from the mouth are signs of bleeding that may be swallowed into the stomach, and then secondarily vomited. A careful history and thorough physical examination will help distinguish between them.
True hematemesis usually indicates a serious underlying disease, and generally warrants hospitalization, extensive diagnostic testing, and supportive care. It is best to determine the underlying cause, and treat the specific problem, rather than solely attempting symptomatic therapy.
Causes for Vomiting Blood in Dogs
Here are the many causes of vomiting in dogs and some specific potential causes for hematemesis. The most common causes are usually diseases or disorders of the upper gastrointestinal tract, although in some cases, clotting disorders (coagulopathies) may result in bleeding even though the gastrointestinal tract is essentially healthy.
Potential Causes of Hematemesis
- Clotting disorders (coagulopathies) that cause bleeding into the gastrointestinal tract. A clotting disorder should be considered, especially if there is evidence of bleeding from other body sites as well. There are many different types of clotting disorders that can cause hematemesis.
- Hemorrhagic gastroenteritis (HGE) is a syndrome seen in dogs whose cause is unknown. The dog usually experiences acute bloody diarrhea, although vomiting and/or hematemesis may be seen as well.
- Vomiting blood that has been swallowed, such as from bleeding in the mouth, nose (epistaxis), coughed up from the lungs (hemoptysis), or licked from the skin.
- Parasitic infections, such as from hookworms, can cause severe symptoms in young pets.
- Viral infections, such as parvovirus, can cause bloody diarrhea and sometimes bloody vomit.
- Gastrointestinal ulcerations or erosions are one of the more common causes of hematemesis. These ulcers can occur with many different disorders, such as:
- The overproduction of stomach acid from stress and certain tumors.
- Infiltrative diseases of the wall of the stomach or upper intestines, such as inflammatory bowel disease.
- Chronic inflammation of the esophagus, especially with regurgitation of acidic stomach contents.
- Chronic inflammation of the stomach, especially from bacteria such as Helicobacter.
- Metabolic diseases, such as kidney failure, chronic liver disease, and Addisons disease.
- Administration of drugs that affect the lining of the stomach, such as nonsteroidal anti-inflammatory agents and corticosteroids.
- Gastrointestinal foreign bodies or tumors, especially of the esophagus, stomach, and upper small intestine.
- Perioperative hemorrhage (bleeding associated with surgical procedures), as in cases of gastrotomy (cutting into the stomach), gastrostomy (creating an opening in the stomach), or repair of a gastric dilatation volvulus (bloat/torsion).
- Heavy metal intoxication with arsenic, lead, or zinc.
- Following anaphylaxis (a severe, life-threatening allergic reaction) or septic shock (due to an overwhelming bacterial infection).
What to Watch For
- Blood in the vomitus. Fresh blood is usually bright red. Old, partially-digested blood is brown and has the appearance of coffee grounds.
- Anorexia
- Diarrhea
- Blood in the feces
- Abdominal pain
- Paleness or pallor of the gums with severe blood loss
- Rapid breathing with severe blood loss
- Weakness, collapse, and shock with severe blood loss
- Signs of bleeding at other sites in or on the body
Diagnosis of Hematemesis in Dogs
Obtaining a complete medical history and performing a thorough physical examination are necessary in order to create an appropriate diagnostic plan for a patient with hematemesis. A history of recent toxin exposure or administration of certain medications may be of paramount importance. Your veterinarian may also recommend the following tests:
- A complete blood count (CBC) evaluates the presence of infection, inflammation, and anemia.
- A biochemical profile helps rule out metabolic causes of hematemesis. It assesses the status of the kidneys, liver, electrolytes, blood proteins, and blood sugar.
- A urinalysis helps evaluate the kidneys and the hydration status of the patient. Additionally, the presence of blood in the urine may help support a diagnosis of coagulopathy.
- A coagulation profile is performed on many patients with hematemesis. It generally includes various clotting tests and a platelet count.
- Abdominal radiographs (X-rays) evaluate the abdominal organs, and may detect the presence of a foreign body, tumor, or chips containing lead.
- Thoracic radiographs evaluate for the presence of fluid or blood in the lungs or chest cavity, the spread of cancer (metastasis), and the presence of esophageal diseases.
- Multiple fecal examinations for parasites and occult blood are important screening tests. Parasites are more likely to cause hematemesis in a young puppy or kitten than in an adult dog or cat.
- A fecal test for parvovirus can confirm the presence of this serious infection.
Additional Testing Options
These are selected on a case-by-case basis:
- An ACTH stimulation test to rule out hypoadrenocorticism (Addisons disease).
- Bile acids to evaluate liver function.
- Measurement of blood lead level.
- Measurement of fasting serum gastrin level, the hormone responsible for increasing gastric acid production.
- An abdominal ultrasound to evaluate the size, shape, and texture of abdominal organs and help assess for the presence of tumors.
- An upper gastrointestinal (GI) barium series to help identify foreign bodies.
- Upper GI endoscopy, which involves passing a flexible viewing scope into the esophagus, stomach, and duodenum, to identify and retrieve foreign bodies or obtain a biopsy.
- An exploratory laparotomy (especially if the cause of the hematemesis remains elusive), which allows for physical examination of the stomach and intestine to identify problems.
Treatment of Hematemesis in Dogs
The vomiting of blood that represents bleeding within the gastrointestinal tract is a serious condition. It generally warrants hospitalization, the performance of numerous diagnostic tests, and at the very least, supportive care. Treatment of severe clinical signs is necessary while diagnostic testing is underway. The following nonspecific (symptomatic) treatments may be applicable to some pets with hematemesis. These treatments may reduce the severity of symptoms or provide temporary relief. Nonspecific therapy is not a substitute for definitive treatment of the underlying disease responsible for your pets condition.
Symptomatic Therapy Options
- No food or drink given by mouth (NPO). Withholding food and water for 12 36 hours allows the GI tract to rest and is important when treating the patient with hematemesis. Complete dietary restriction allows the lining of the GI tract to heal. Gradual reintroduction of small amounts of bland food is instituted after the fast. Once all vomiting and hematemesis have resolved, the original diet may be slowly reintroduced. If at any point clinical signs recur, discontinue all oral food and water and contact your veterinarian.
- Intravenous (IV) fluid and electrolyte therapy. Fluid and electrolyte therapy may be necessary and are directed toward correcting dehydration, acid-base, and electrolyte abnormalities. Occasionally, subcutaneous (under the skin) administration is adequate, and may be performed on an outpatient basis. In more severe cases, IV administration is indicated and necessitates hospitalization.
- Blood transfusions may be indicated if your pet is anemic from continued blood loss and hematemesis.
- Drugs that stop vomiting (antiemetic) are used with caution. It is best to identify and treat the underlying cause of hematemesis, although in selected cases these medications may be recommended.
- Gastric acid blocking agents and gastric protectant drugs to treat for gastrointestinal ulceration while awaiting test results. Drugs that decrease or inhibit acid production by the stomach, such as Tagamet (cimetidine), Pepcid (famotidine), Zantac (ranitidine), and Prilosec (omeprazole), may encourage and expedite the resolution of hematemesis, especially if it is related to gastrointestinal ulcers.
- Medications that protect or sooth the lining of the esophagus, such as sucralfate (Carafate).
- Antibiotics
- Prostaglandin drugs, such as misoprostol (Cytotec), may help counteract the ulcerogenic effects of nonsteroidal anti-inflammatory drugs (NSAIDs).
- In some cases, surgical intervention is recommended, especially where a hemorrhage is uncontrolled, a bleeding ulcer has perforated the gastrointestinal tract, or a bleeding tumor is present.
Home Care and Follow-up Care for Dogs with Bloody Vomit
- Call your veterinarian immediately if there is blood present in the vomitus.
- It is important to administer all medications and follow dietary recommendations as directed by your veterinarian. Alert your veterinarian if you are experiencing problems treating your pet.
- Avoid drugs that might damage the gastrointestinal tract, such as corticosteroids and other anti-inflammatory drugs.
Optimal treatment for your pet requires a combination of home and professional veterinary care. Follow-up evaluations are critical, especially if your pet does not rapidly improve.
Prevention Tips
- Never give a steroid, such as prednisone, with an anti-inflammatory drug. This combination can cause bleeding ulcers.
- Minimize your pets exposure to molds, garbage, and trash.
- Provide safe chew toys that cannot be ingested.
- Learn about the 21 Symptoms You Should Never Ignore in Your Dog.
FAQs About Vomiting Blood in Dogs
Some frequently asked questions about vomiting blood include the following:
Is a little blood in vomit normal?
Blood in the vomit is never normal. If you see this abnormal symptom in your dog, please call your veterinarian or local veterinary emergency clinic.
When is a dog vomiting an emergency?
Vomiting in dogs is an emergency if your dog is lethargic, weak, not eating, or when the vomiting is not productive.
What should I do if my dog throws up blood?
If your dog vomits blood, call your veterinarian. Read the above information on possible causes and treatments.
What causes my dog to cough blood?
Coughing up blood, also known as hemoptysis, can be caused by infections, bleeding disorders, toxins, heart failure, and tumors. It is always abnormal.
What could cause my dogs vomit to be black?
Black vomit is caused by ingestion of something black (such as pigmented mulch) or from vomiting of digested blood (often resembling coffee grounds).
This can occur due to bleeding disorders, liver disease, bleeding ulcers, and conditions such as Hemorrhagic Gastroenteritis.
Please see your veterinarian if you notice any abnormal symptoms in your dog to determine the best options for treatment.
Kidney Disease in Dogs: Signs, Symptoms, and Treatment
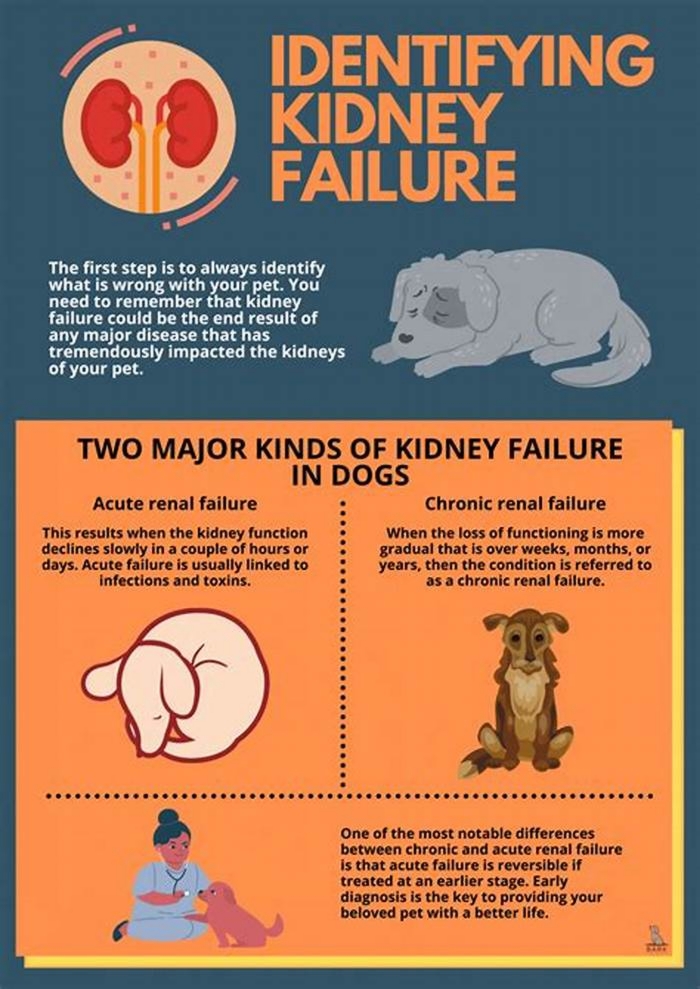
Your dogs kidneys are essential organs that filter waste products from the bloodstream. When the kidneys are weakened, either by acute or chronic kidney disease, your dogs health could suffer. Because kidney disease progresses over time, its important to learn the common symptoms so tha you can recognize them. If you catch kidney disease in dogs early on, treatment can slow down the progression and allow your dog to live longer.
What Is Kidney Disease in Dogs?
Kidney disease in dogs is sometimes called renal or kidney insufficiency because it occurs when a dogs kidneys stop doing their job as efficiently as they should. The main job of the kidneys is to help clear and excrete waste products from the blood and convert them to urine, says Dr. Jerry Klein, Chief Veterinary Officer for the AKC. If the kidneys are not working properly, these waste products can build up in the blood, causing detrimental effects.
Dogs can get either acute kidney disease, which develops suddenly, or chronic kidney disease (CKD), which develops slowly and worsens over an extended period. Both involve loss of kidney function, but they result from different circumstances. Acute kidney disease is a sudden attack or injury to the kidney, whereas chronic kidney disease is a slow, degenerative loss of kidney function, Dr. Klein explains.
What Causes Kidney Disease in Dogs?
Dr. Klein warns that kidney disease could be caused by a lot of things, including infection (such as with the bacteria that causes leptospirosis), trauma, genetics, drugs, toxins, cancer, mechanical obstructions (like kidney stones), and degenerative diseases (where the job and form of the affected body part get worse over time). Anything that decreases blood flow to the kidneys, such as dehydration or heatstroke, can cause the kidneys to fail.
Acute kidney disease in dogs can be caused by exposure to hazardous materials, including toxic plants such as lilies, certain drugs, harmful foods such as grapes or raisins, or antifreeze. Puppy-proofing your home and yard can keep your dog away from potentially harmful items or foods that could be toxic.
Chronic kidney disease in dogs is also associated with growing older. Because kidney tissue cant regenerate once its damaged, the kidneys can wear out over time. As small-breed dogs often live longer than large-breed dogs, they tend to show early signs of kidney disease at an older age10 years old or more, compared to as young as 7 for the large breeds.
What Are the Symptoms of Kidney Disease in Dogs?
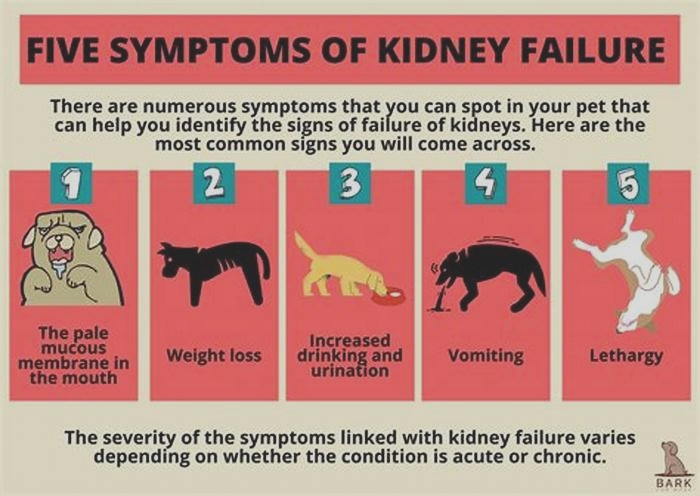
The earliest signs of kidney disease in dogs are increased urination and therefore increased thirst. Other symptoms dont usually become apparent until about two-thirds of the kidney tissue is destroyed. So, in the case of CKD, the damage may have begun months or even years before the owner notices. Because of this, its common for the signs of kidney disease in dogs to seem like they came out of the blue when in fact, the kidneys have been struggling for a long time.
Other signs of chronic kidney disease in dogs to watch for include:
Dr. Klein says there are some rarer symptoms of kidney disease in dogs to be aware of, as well. On occasion, there can be abdominal painurinary obstructions or stonesand in certain instances, one can see ulcers in the oral or gastric cavity. In extreme cases, little or no urine is produced at all.
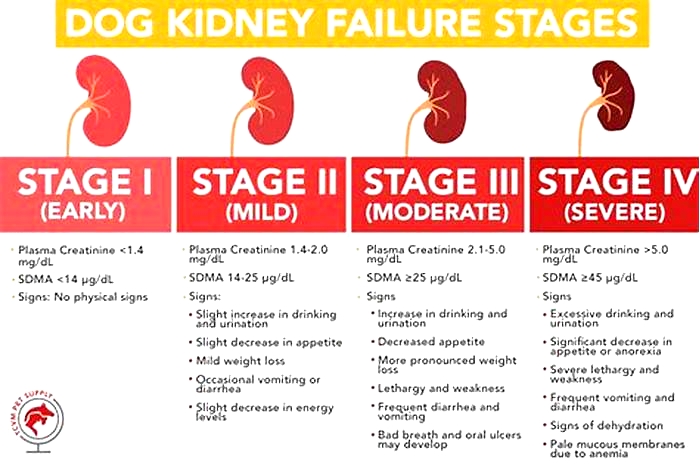
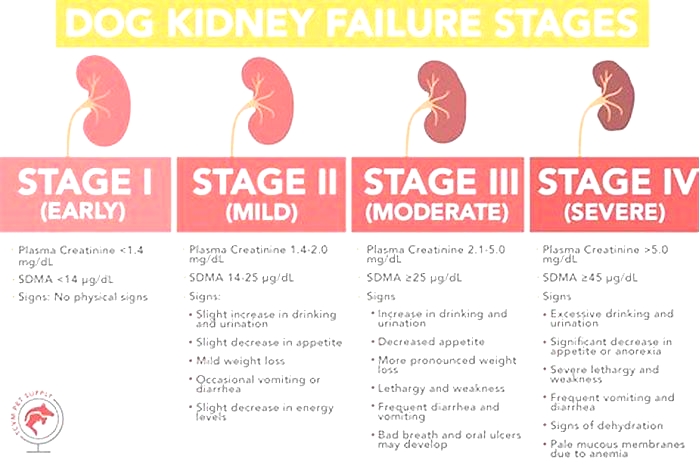
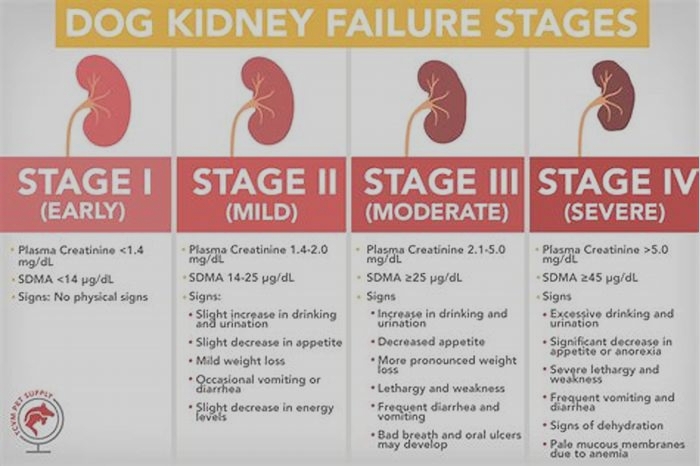
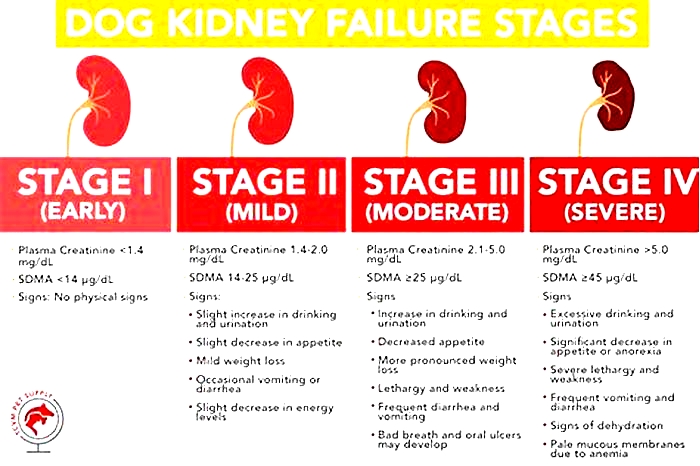
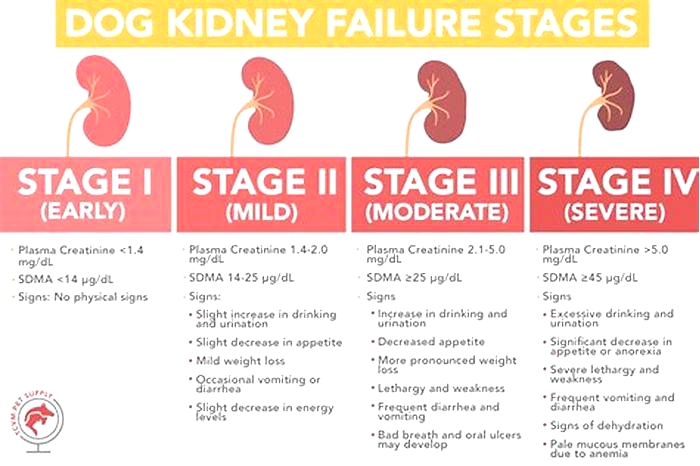
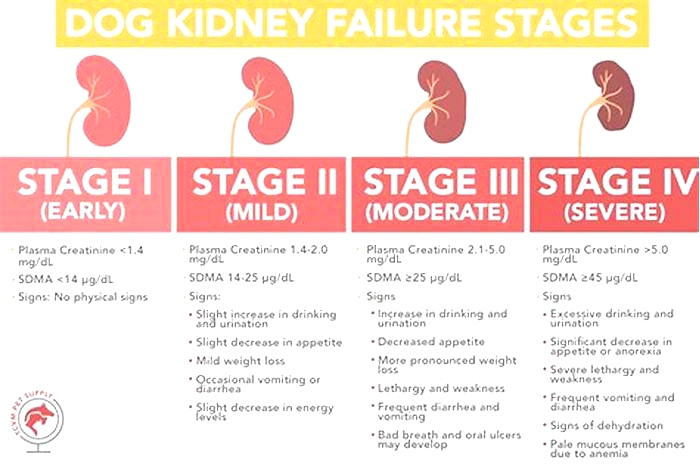
What Are the Stages of Chronic Kidney Disease in Dogs?
Kidney disease in dogs is measured in stages. Many veterinarians use the IRIS scale, which has four stages. Blood work measurements like creatinine and SDMA (biomarkers for kidney function) allow your vet to assign your dog to a particular stage which will determine the exact treatment.
Dr. Klein explains, The stages determine how well the kidneys can filter waste and extra fluid from the blood. As the stages go up, the kidney function worsens. In the early stages of CKD, the kidneys are still able to filter out waste from the blood. In the latter stages, the kidneys must work harder to filter the blood and in late stages may stop working altogether.
How Is Kidney Disease in Dogs Treated?
Dialysis (a medical procedure that removes waste products and extra fluid from the blood) is far more common in humans than in dogs, although peritoneal (kidney) dialysis can be performed in some cases. On rare occasions, surgical kidney transplant is possible in dogs.
But Dr. Klein specifies that depending on the type and stage of kidney disease, the main treatments for CKD are diet changes and administration of fluids, either directly into the veins (intravenous) or under the skin (subcutaneous). The balancing and correction of electrolytes are extremely important in the management of kidney patients, he explains.
Proper nutrition is needed, and there are many available diets formulated for cats and dogs with kidney issues, some by prescription only. Your veterinarian can help guide you to the most appropriate diet for your pet.
Because kidney disease, particularly in the late stages, can cause a dog to lose their appetite, it can be difficult to encourage your dog to eat enough. Dr. Klein advises, There are medications used as appetite stimulators available, such as the prescription drug mirtazapine. Capromorelin has recently been FDA-approved for dogs to address appetite in chronic kidney disease.
When Do You Need to Call Your Vet?
The prognosis and expected life span for a dog with kidney disease depend on the type of disease, the speed of progression, and underlying conditions present in the dog. However, the more serious the disease, the poorer the outcome. Thats why its so crucial to catch the illness early on.
According to Dr. Klein, In chronic kidney disease, there are methods, such as diets and medications, that can be used to lessen the burden of work the kidneys need to do and may help slow down the progression from one stage to the next. In acute kidney disease, there is less time and fewer choices available to prevent further damage to the kidneys and to try to jump-start the kidneys to get them to function normally.
Regular veterinary exams, including bloodwork, are an excellent way to spot kidney problems before the outward symptoms become apparent. And if you notice any of the above signs, dont hesitate to get your dog to the vet for further testing. It can make a huge difference in preserving kidney function and your dogs well-being for as long as possible.