dog kidney failure rapid breathing
Rapid, shallow breathing (not panting) while at rest
Last night after our last walk, Honey was lying down in front of a fan in my room (it's hot here, AC is also on, but she really likes the fan), and breathing very rapidly (80 breaths per minute). The breathing was shallow. Her temperature was normal (101.7), gums and eyes were normal, and she didn't seem to be in distress or pain in any other way.
She was not sleeping at first, but then she dozed off. The breathing went on like this for over an hour. I fell asleep, then woke up in the middle of the night and checked on her and all was back to normal; she was taking about 18-22 breaths/minute. She was fine this morning, and I watched her very closely after we got back from our walk, and she was tired, but her breathing was normal while she was lying down.
We were out of town visiting family last week, and just got home yesterday, so she has had a lot going on. She was very tired yesterday and this morning, but I expected that since she has been so active recently.
Also, she has been quite itchy since the end of last week because she was outside a lot and seems to have gotten bug bites (I was with her and I have a lot of bug bites, too). She is on Frontline Plus, but I have learned that Frontline doesn't protect against bugs (thinking about switching to K9 Advantix). I don't know if the breathing is related to the itching.
Lastly, she has had a few minor sneezing episodes (2-3 sneezes per episode, 1-2 times each day) over the past day or two. I assumed it was just allergies, because she is a pretty allergic dog and we were in a new environment, but perhaps this is related to the breathing, too?
Anyway, what could cause this type of breathing? I'm concerned because when I look up information about rapid, shallow breathing at rest, it points to heart or kidney failure, but she is not showing other symptoms of either at the moment. And she is only about 3 years old
We have a vet appointment this Thursday (7/12) to recheck blood work for an issue (fever/lethargy, with strange results on her blood work) that had us at the vet 3 weeks ago, so I would rather not go in before then unless it's an emergency, but was wondering if anyone had any experience with this? Is it normal? If not, what could it point to? Are there any questions I should ask the vet/tests we should run?
Signs of a Dog Dying of Congestive Heart Failure (CHF)
Congestive heart failure (CHF) is when the heart isnt able to pump blood adequately throughout the body. This results in blood backing up into the lungs and fluid accumulating in the body cavities, which constricts the heart and lungs and prevents sufficient oxygen flow throughout the body.
In most cases of CHF, the issue is not reversible. Here are some of the signs that your dog might be nearing a stage where they need hospice care or you would consider euthanasia.
What Are the Signs of a Dog Dying of Congestive Heart Failure?
There are several stages of congestive heart failure:
- Stage A: The dog is high-risk for CHF, but has no symptoms and no changes to the heart.
- Stage B1: The dog has a heart murmur but no other signs.
- Stage B2: The dog has a heart murmur in addition to structural changes to the heart, but no clinical signs.
- Stage C: The dog has a heart murmur, structural changes to the heart, and clinical signs associated with CHF. These dogs are typically treated.
- Stage D: The dog has CHF and is not responding to standard therapies. The dog will require special treatment strategies.
The clinical signs for CHF are similar once a dog reaches Stage C and D. These clinical signs that a dog is dying of congestive heart failure are:
If you see these signs of late-stage CHF, it does not mean you must immediately consider euthanasia. A pets symptoms can resolve or be managed at a variety of stages.
For example, cough, trouble breathing, and rapid breathing may be treated with bronchodilators, antibiotics, corticosteroids, cough suppressants, environmental modification (air purifiers), and even weight loss.
Monitoring Your Dogs Quality of Life With Late-Stage CHF
As CHF progresses into the hospice/palliative care stages (starting at Stage C), your veterinarian will focus on maintaining your dogs quality of life. Some questions that your vet may consider and discuss with you include:
Can the dog breathe comfortably on their own?
Does the dog enjoy meals?
Does the dog enjoy interactions with their family?
Can the dog get around to pee and poop with dignity and rest comfortably?
Its important to check in regularly with the veterinary team to help maintain your dogs quality of life. Possible complications can come up as a result of disease progression or a side effect of medication. Some of these complications have signs you can see, but others will only show up in lab work at the vets office. These may include:
Lack of appetite
Pulmonary edema (fluid in the lungs)
Ascites (swollen belly from fluid in the abdominal cavity)
Gastrointestinal ulceration
Anxiety
Diarrhea
Weight loss and muscle mass loss
Changes in electrolyte blood work values:
Hypochloremia (low blood chloride)
Hyponatremia (low sodium in blood)
Hypokalemia (low potassium in blood)
Hyperkalemia (high potassium in blood)
Kidney disease/failure
When Should You Euthanize a Dog with Congestive Heart Failure?
The decision to euthanize a pet that has congestive heart failure is a very difficult and personal choice. While input from your dogs vetsuch as blood work values, physical exam findings, and costare all important to consider, your dogs quality of life and your own concerns are also important factors that can vary greatly.
You know your pet best, and you also know what you are capable of doing for your pet. You also know when your pet seems to be having a really hard time. So when it comes to answering the question, Is it time? the answer for your pet may be different from someone elses pet, even if they are in a similar situation.
Your veterinary team is there to help you and your pet by giving support in any way they can. There is no shame in letting your pet go when a diagnosis is reached. Nor is there any shame in supporting your pet until there may be more bad days and good.
Quality of life checklists can be very helpful in giving a more objective outlook, and you can review these with your vet to get a clearer picture. Lap of Love has some great resources for this:
You can also use this Quality of Life Scale by Dr. Alice Villalobos to evaluate your pet:
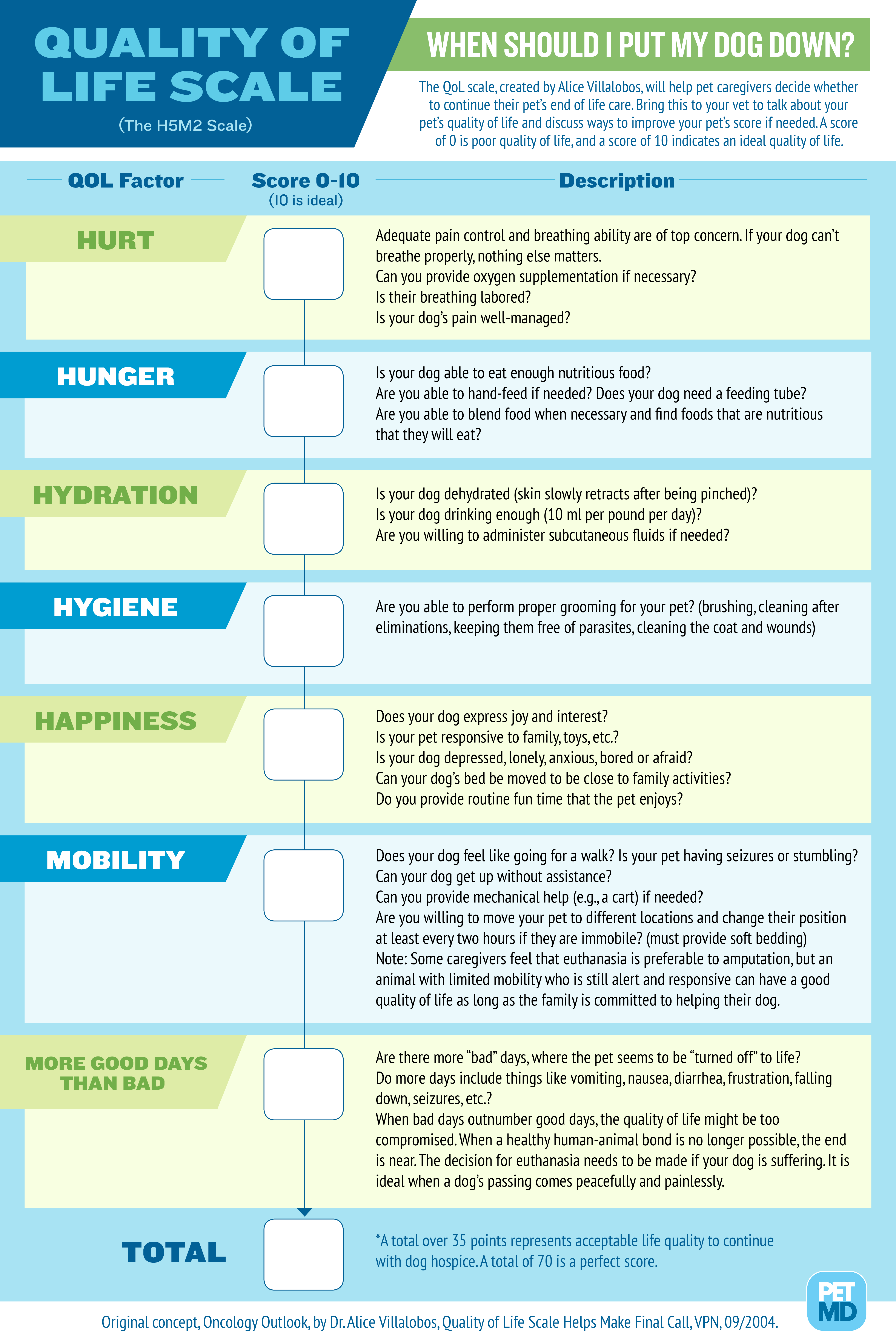
Because every experience is different, it may be helpful to create your own quality of life checklist and discuss it with your dogs vet as well as any family members, friends, and others who are involved in your pets care. This will help make sure the list is reasonable and true to the needs of both you and your pet.
If youd like to talk to a vet about how to evaluate your pets quality of life or have questions about CHF stages, and you have an account with Chewy, you can chat now with licensed veterinary experts through Chewys Connect with a Vet service, or you can schedule a video call.
Featured Image: iStock.com/capuski
Managing Kidney Failure in Dogs
Kidney failure in dogs can seem like a devastating diagnosis. If you've been told by your veterinarian that your dog has a kidney problem that might end in kidney failure one day, don't lose hope. Depending on the circumstances, that day may be farther off than you think. With that note in mind, here are a few things you should know.
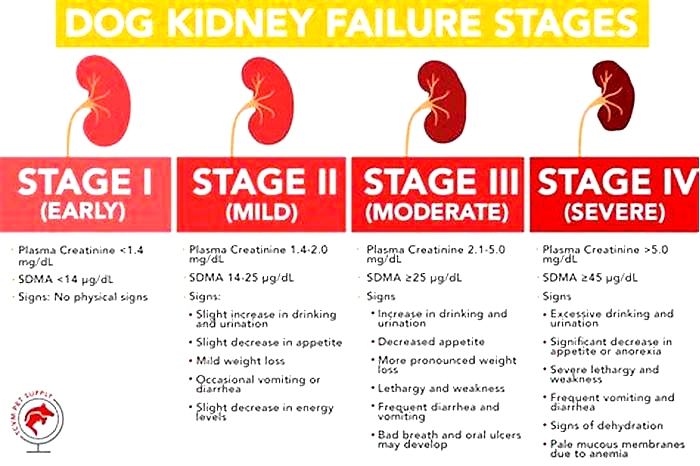
Identifying Kidney Failure in Dogs
Kidney failure (also known as renal failure) is the end result of any one of a large number of diseases that can affect the kidneys and related organs. Technically, it occurs when the kidneys can no longer efficiently perform their function, which is to filter out toxins, maintain a normal electrolyte balance, regulate hydration, and secrete hormones needed for the production of red blood cells.
There are two broad types of kidney failure in dogs:
- Acute renal failure: When kidney function suddenly declines (in hours or days), the process is referred to as acute. Acute renal failure in dogs is most commonly associated with infections and toxins.
- Chronic renal failure: When the loss of function is more gradual (over weeks, months or years), it's called chronic renal failure. The most common cause of chronic renal failure in dogs is degeneration associated with geriatric decline. All kidneys have their own natural lifespan, but some dogs' kidneys deteriorate more quickly than others.
One of the most notable differences between acute and chronic kidney failure is that acute kidney failure is reversible if treated early and aggressively, whereas chronic kidney failure can only be managed.

The Causes of Kidney Failure
Kidney failure is ultimately caused by any disease affecting the kidneys. These include:
- Bacterial infections, like leptospirosis, which the Centers for Disease Control and Prevention reports can be transmitted by drinking or swimming in contaminated water. This infection can lead to inflammation of the kidneys and consequent destruction of renal cells.
- Toxicosis, or kidney poisoning, leads to damage of the kidneys' cells. It occurs when your dog ingests drugs (like ibuprofen) or poisons (like antifreeze or grapes). The ASPCA's Animal Poison Control Center lists these and other common household items that should be kept out of your dog's reach.
- Congenital disease: Inherited conditions can lead to abnormal kidney function. The Merck Veterinary Manual includes a list of these congenital diseases, from cysts to agenesis (being born without one or both kidneys).
- Geriatric degeneration: When kidneys get old, their cells can decline and die. This is, by far, the most common cause of kidney disease in dogs.
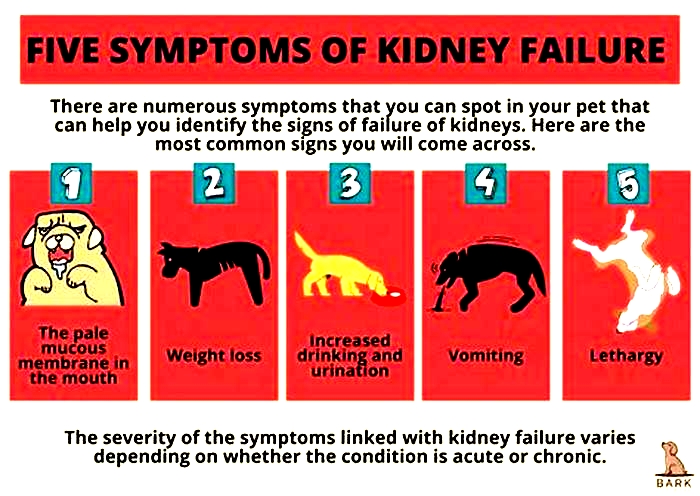
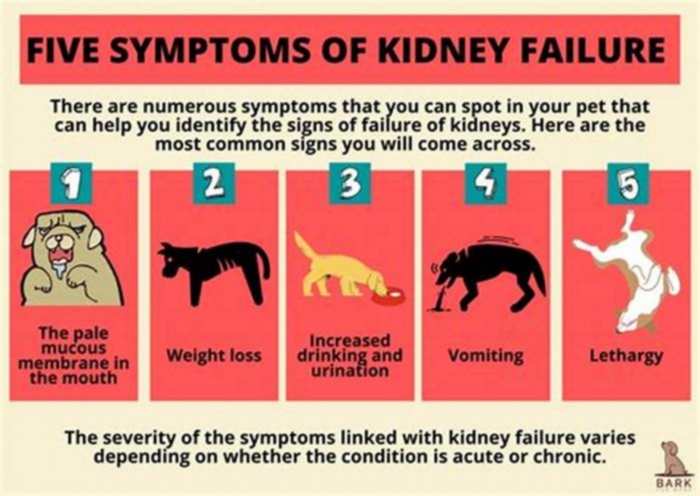
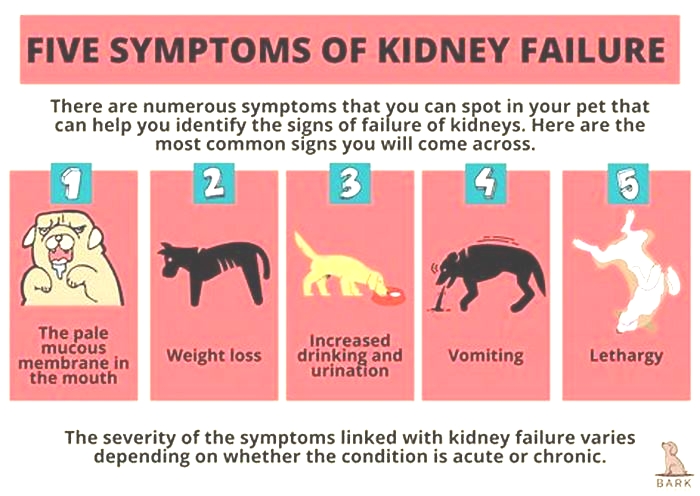
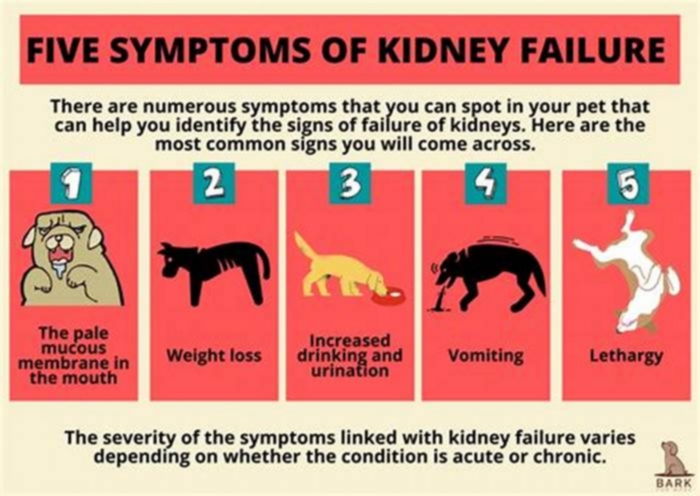
Symptoms of Kidney Failure
The most common signs of kidney failure in dogs include:
- Vomiting
- Increased drinking and urination
- Lethargy
- Weight loss
- Pale mucous membranes in the mouth and elsewhere
The severity of clinical signs associated with kidney disease can vary depending on the presentation (acute or chronic), the extent to which the loss of kidney function has progressed and the underlying cause. Your vet can determine whether these signs point to a kidney problem or another issue, like diabetes mellitus.
Treating Kidney Failure in Dogs
The treatment of kidney failure varies depending on the underlying cause and the canine patient's overall condition. Dogs that are severely ill from acute kidney failure may need hospitalization and intensive care to recover. For milder cases, antibiotics, fluids, and other medications given on an outpatient basis can prove effective. Dialysis is even a possibility for a lucky few whose pet parents can afford the high cost of treatment.
In the case of chronic renal failure in dogs, treatment generally focuses on slowing the progression of disease and improving quality of life for the patient. Treatment of anemia, blood pressure alterations, electrolyte disturbances, fluid imbalances, nausea, and appetite changes is typically necessary. Most of these signs are managed through diet changes and medication. Pets can sometimes experience a good quality of life for years after a kidney failure diagnosis.

Preventing Renal Failure
Given that chronic renal failure in dogs is most commonly the result of genetically predetermined, age-related degeneration, it's not considered preventable. Nonetheless, regular physical examinations and wellness screenings can increase your dog's chances of early diagnosis and treatment.
Acute renal failure, however, is considered preventable in many instances. Vaccination against infectious diseases, like leptospirosis, for example, can prove highly effective. Clearing households of toxins, like antifreeze; being careful with grapes and raisins; and keeping all human medications out of the reach of dogs is also important.
Understanding Your Dog's Risk
The timing of kidney degeneration is likely linked to a dog's genetics. Consequently, chronic renal failure in dogs is effectively preprogrammed to occur at a certain age. Nonetheless, no specific breed predisposition is known to exist. Certain kidney diseases that can lead to renal failure in dogs, however, can disproportionately affect specific breeds. These include the following:
- Basenji dogs are especially affected by Fanconi syndrome, which disrupts electrolyte absorption.
- Bernese mountain dogs can suffer a congenital disease of the kidneys called glomerulonephritis.
- Collies, Shetland sheepdogs and German shepherds can be affected by lupus, an autoimmune disease affecting the kidneys and other organs.
- Shar-Peis can suffer a kidney disease known as familial renal amyloidosis.
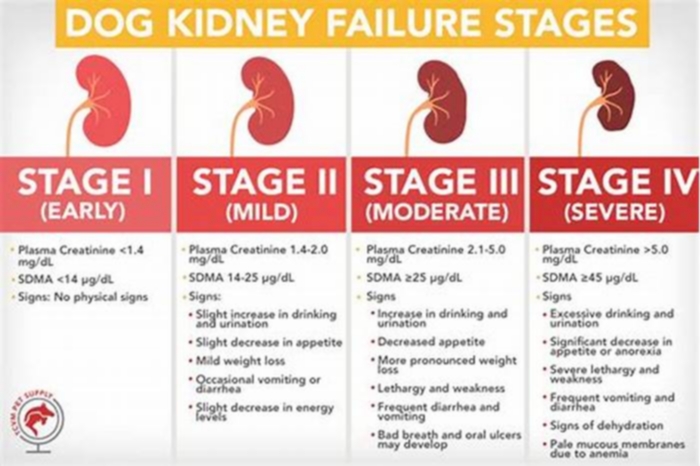
It can prove difficult to determine which dogs will suffer these conditions in advance. New blood tests, however, are now helping identify kidney disease in dogs and cats early, sometimes even many years before signs become evident. One test called the SDMA (which IDEXX notes is named for symmetric dimethylarginine, a genetic marker for kidney function) is now considered very common. Many veterinarians consider it part of their annual wellness screening; be sure to ask your vet if this test is available for your dog at your next appointment.
The Role of Nutrition
Nutrition has long been a mainstay in the management of renal failure in dogs. Since maintaining electrolyte balance and managing blood proteins are a crucial part of the kidneys' role, altering the nutrients in a dog's diet can make kidney function easier. All dog parents whose pets suffer from kidney disease should talk to their veterinarian about the ideal therapeutic diet and any additional nutritional supplements that might be in order.
Dog parents have so many more options than ever before when it comes to treating and managing renal failure. Given advances in nutrition and drugs, the longevity of veterinary renal patients is most definitely on the rise. With your veterinarian's assistance, a long life for your pup is a possibility.
Contributor Bio

Dr. Patty Khuly
Dr. Patty Khuly is an honors graduate of both Wellesley College and the University of Pennsylvania School of Veterinary Medicine. She received her MBA at The Wharton School of Business as part of the prestigious VMD/MBA dual-degree program. She's now the proud owner of Sunset Animal Clinic in Miami, Florida. But that's not all. Dr. K is a nerdy reader, avid knitter, hot yoga fanatic, music geek, struggling runner, and indefatigable foodie. She lives in South Miami with three dogs, countless cats, two rescued goats and a hilarious flock of hens.
You can follow her writing at DrPattyKhuly.com and at SunsetVets.com.